Neuroma Treatment in New Jersey
The Foot & Ankle Center
at Modern Orthopedics of New Jersey
Paramus
72 Route 17 North
Paramus, NJ 07652
Wayne
2025 Hamburg Turnpike
STE C, Wayne, NJ 07470
Parsippany
3799 US-46
#207, Parsippany, NJ 07054
Neuromas are benign growths or thickened areas of nerve tissue that typically develop due to repetitive trauma or compression of a nerve. They commonly occur in the feet, particularly between the metatarsal bones. Neuromas result in symptoms such as pain, tingling, numbness, or a burning sensation in the affected area. The discomfort often worsens with activity or pressure on the affected nerve. In Morton’s neuroma, a specific type of neuroma affecting the nerves between the third and fourth toes (anatomically in between 3rd and 4th metatarsal heads), individuals may experience the sensation of a pebble or lump in their shoe. These symptoms can significantly impact daily activities and prompt individuals to seek medical attention for symptom relief and pain management.
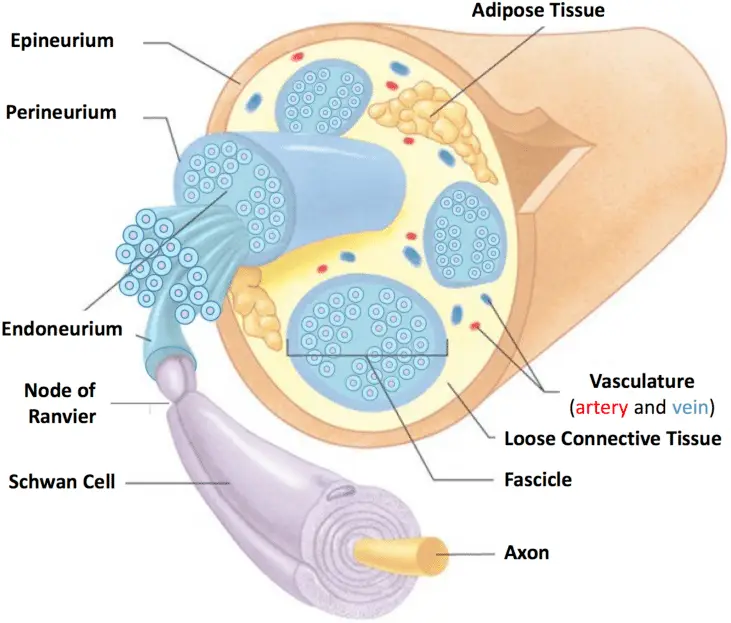
Below is a diagram of healthy nerve anatomy:
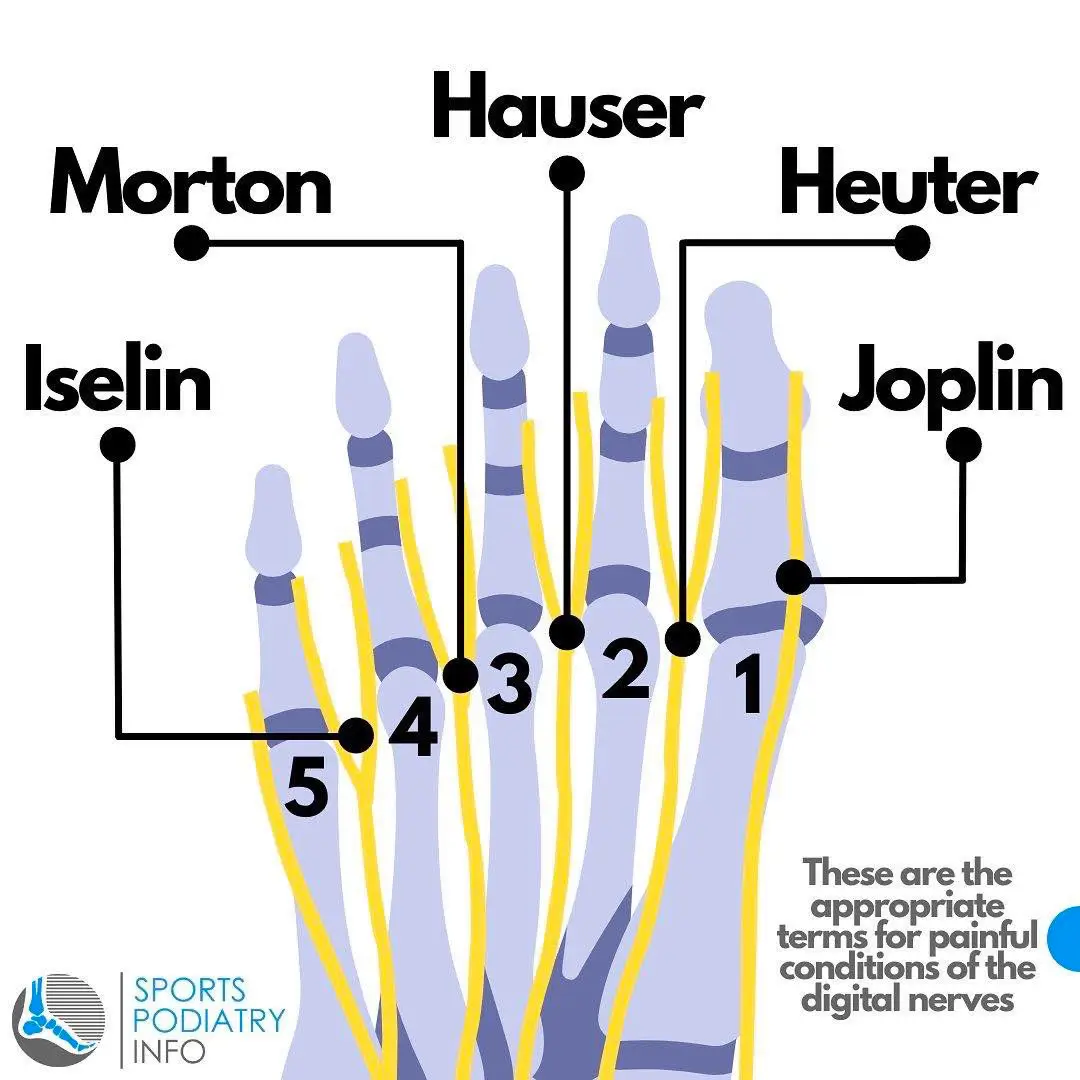
This is a helpful diagram to illustrate the different neuromas of the forefoot located in the intermetatarsal spaces:
Diagnosing a Neuroma
In a physical examination for diagnosing neuroma, a healthcare professional will typically:
- Palpate the affected area, usually the foot, to locate areas of tenderness or a palpable mass.
- Apply pressure between the metatarsal bones to reproduce symptoms such as pain, tingling, or numbness.
- Assess for any changes in sensation or muscle strength in the affected area.
- Evaluate gait and observe for any abnormalities in foot mechanics that may contribute to the development of neuroma.
- Perform specialized maneuvers, such as Mulder’s sign (a click felt when compressing the affected area), which can be indicative of Morton’s neuroma specifically.
Based on the findings of the physical examination, along with the patient’s reported symptoms and medical history, the healthcare professional can make a preliminary diagnosis of neuroma and may recommend further diagnostic tests, such as imaging studies, to confirm the diagnosis and guide treatment.
Imaging Tests:
- Ultrasound: Ultrasound imaging can provide real-time images of the affected area, allowing the physician to visualize any abnormalities, such as the presence of a neuroma. It is particularly useful for evaluating soft tissue structures like nerves. However, the challenge of an ultrasound study is that it is highly user-dependent.
- Magnetic Resonance Imaging: MRI is highly effective in identifying neuromas and assessing their size, location, and relationship to surrounding tissues. MRI is often preferred when further detail is required or when other imaging modalities are inconclusive.
Diagnosing neuromas typically involves a combination of clinical evaluation and imaging tests. A healthcare professional will conduct a physical examination, assess symptoms, and review medical history. Imaging tests may be used to confirm the diagnosis and get a more detailed assessment. This comprehensive approach helps ensure an accurate diagnosis, allowing for appropriate treatment planning and management of the condition.
Importance of Seeking Treatment for Neuromas
Seeking treatment for neuromas is crucial to alleviate symptoms and improve quality of life. Left untreated, neuromas can lead to chronic pain, discomfort, and limitations in daily activities. Effective management strategies, including conservative measures like rest, orthotic devices, and physical therapy, can help relieve symptoms and prevent further progression of the condition. In severe cases, surgical intervention may be necessary to remove the neuroma or release pressure on the affected nerve. Early diagnosis and prompt treatment can significantly reduce the impact of neuromas, enabling individuals to maintain active lifestyles and minimize long-term complications.
Understanding Neuroma Treatments
Neglecting treatment for neuromas can lead to chronic pain, discomfort, and decreased mobility. Without intervention, symptoms may worsen over time, impacting daily activities and quality of life. Delaying treatment may also increase the likelihood of requiring more invasive interventions later on. In rare instances, non-treatment can lead to the development of pain syndromes when left untreated.
Consulting with a healthcare professional for proper diagnosis and treatment planning for neuroma is essential for accurate diagnosis, individualized treatment plans, access to resources, monitoring and follow-up, patient education, and safety management. Healthcare professionals possess the expertise and resources to accurately diagnose neuroma through thorough examinations and diagnostic tests, tailoring treatment plans to address specific patient needs while coordinating with other healthcare providers for comprehensive care. Regular monitoring and follow-up ensure treatment effectiveness and allow for adjustments as needed, while patient education empowers individuals to participate in their healthcare decisions. Additionally, healthcare professionals assess treatment risks and implement safety measures, minimizing potential complications and ensuring the best possible outcomes for patients.
Non-Surgical Treatment Approaches
Non-surgical treatment approaches for neuromas aim to alleviate symptoms and improve quality of life. These may include:
Therapy
- Orthotic Devices: Custom-made with specialized offloading modifications that serve as shoe inserts can help redistribute pressure and reduce irritation on the affected nerve.
- Footwear Modifications: Wearing shoes with a wider toe box or low heels can relieve pressure on the forefoot and alleviate symptoms.
- Padding and Taping: Padding or taping the affected area can provide cushioning and support, reducing friction and irritation on the nerve.
- Physical Therapy: Stretching and strengthening exercises can improve foot mechanics, reduce inflammation, and alleviate pain associated with neuromas.
Medications
- Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce pain and inflammation.
Cortisone Injections
- Corticosteroid injections can provide temporary relief by reducing swelling around the affected nerve.
More Helpful Tips:
- Ultrasound Therapy: This non-invasive treatment uses high-frequency sound waves to promote tissue healing and reduce pain and inflammation in the affected area.
- Ice Massage: Applying ice to the affected area can help reduce swelling and alleviate some pain associated with neuromas.
- Activity Modification: Avoiding activities that exacerbate symptoms, such as prolonged standing or high-impact exercises, can help prevent further irritation of the affected nerve.
These non-surgical approaches are often effective in managing symptoms and improving function for individuals with neuromas. However, the choice of treatment depends on the severity of symptoms, individual preferences, and the response to conservative measures.
Surgical and Other Procedures
Decompression Surgery
Decompression surgery is a surgical approach used to treat neuromas by relieving pressure on the affected nerve. During the procedure, the surgeon creates additional space around the nerve, alleviating compression and reducing irritation. This may involve releasing tight ligaments (the intermetatarsal ligament, for example) or removing nearby structures that contribute to nerve compression. Decompression surgery aims to provide long-term relief from symptoms such as pain, numbness, and tingling associated with neuromas, particularly when conservative treatments have been ineffective. While decompression surgery is generally less invasive than nerve removal procedures, it still carries risks such as infection, nerve damage, or incomplete relief of symptoms. Therefore, it’s crucial for patients to discuss the potential benefits and risks of decompression surgery with their healthcare provider before proceeding with treatment.
Patients undergo anesthesia, and the surgeon makes small incisions to access the compressed nerve. After surgery, patients are monitored before discharge. Recovery involves rest, pain management, and a gradual return to activities. Follow-up appointments ensure proper healing and symptom improvement. While recovery times vary, most experience relief post-surgery. Communication with healthcare providers is crucial throughout the process.
Nerve Removal
Surgical removal of the neuroma may be necessary when conservative treatments fail to provide relief or when the neuroma causes severe and persistent symptoms that significantly impair the patient’s quality of life. These symptoms may include severe pain that limits daily activities, persistent numbness or tingling, or motor dysfunction affecting movement or coordination. Additionally, if the neuroma continues to grow despite non-surgical interventions, surgical removal may be recommended to prevent further complications. The decision to proceed with surgery is made on a case-by-case basis, taking into account the severity of symptoms, the patient’s overall health, and their preferences. During the procedure, the remaining ends of the nerve are capped with specialized material, buried in bone or muscle to prevent the formation of a stump neuroma, which can otherwise be painful.
Potential Risks and Benefits of the Procedure
The surgical removal of a neuroma carries inherent risks and potential benefits. Risks include the possibility of infection, nerve damage, stump neuroma formation, scarring, persistence of symptoms post-surgery, and rare complications such as excessive bleeding or adverse reactions to anesthesia. Conversely, benefits may include relief from symptoms such as pain, numbness, and tingling, as well as improved function and mobility in the affected area. Surgical removal can also prevent further complications and enhance the patient’s overall quality of life by restoring their ability to engage in daily activities without discomfort. Patients should weigh these factors carefully and consult with their healthcare provider to make an informed decision regarding the procedure.
Long-term Effects and Possible Numbness in the Affected Area
Long-term effects of neuroma surgery can include residual numbness or altered sensation in the affected area. Despite successful removal of the neuroma, nerve damage or disruption during surgery may lead to persistent numbness or changes in sensation. This numbness or altered sensation may gradually improve over time as the nerves regenerate and heal, but in some cases, it may persist indefinitely. Patients should be aware of this potential outcome and discuss it with their healthcare provider during the decision-making process. It’s essential for patients to follow post-operative care instructions carefully and communicate any concerns or changes in sensation with their healthcare provider to ensure appropriate management and monitoring of long-term effects.
Preparing for Your Appointment
Preparing for a medical appointment related to neuroma treatment involves several key steps. First, jot down your symptoms and questions to ensure you cover all concerns during the appointment. Bring along any relevant medical records, including past treatments and medication lists. Consider your treatment goals and any specific concerns you have about your condition. If needed, bring a friend or family member for support and assistance. Wear comfortable clothing and bring along the shoes you typically wear, as these may be relevant to your discussion. During the appointment, be open and honest with your healthcare provider about your symptoms and lifestyle. Take notes or record the conversation to remember important details and follow-up instructions. Finally, discuss a follow-up plan with your provider before leaving the appointment. These steps can help ensure a productive and informative visit with your healthcare provider regarding your neuroma treatment.
What To Expect During the Appointment Process
During the appointment process for neuroma treatment, you’ll check in, have vital signs taken, and meet with your healthcare provider. They’ll examine you, discuss symptoms and treatment options, possibly order tests, and collaborate with you on a treatment plan. Expect to ask questions and receive instructions for follow-up care.
Questions To Ask Your Doctor or Specialist
Here are the top five questions to ask your doctor or specialist during a neuroma treatment appointment:
- What are the treatment options available for my neuroma, and which do you recommend for my specific case?
- What are the potential risks and benefits associated with each treatment option?
- What is the expected outcome of the recommended treatment, and how long will it take to see results?
- Are there any lifestyle modifications or self-care measures I can take to manage my symptoms?
- What is the long-term prognosis for my condition, and how often should I follow up with you for monitoring and evaluation?
These questions can help you gain a better understanding of your condition, treatment options, and what to expect moving forward in your neuroma treatment journey.



A Different Orthopedic Experience.
We combine cutting-edge technology with personalized care to deliver exceptional orthopedic treatment. Our team of experts focuses on your unique needs to ensure optimal outcomes and a superior healing experience.
Our Approach to Care
Comprehensive solutions for your orthopedic needs
Treatment Diversity
We offer a comprehensive range of treatments, ensuring personalized, targeted plans for every patient.
Technological Excellence
We utilize cutting-edge technology for precise diagnosis and innovative treatment options.
Collaborative Care
Our multi-disciplinary approach involves various specialties to provide comprehensive care and recovery.
Skilled Experts
Our team is composed of highly skilled, experienced orthopedic professionals, providing expert care.
Patient Focus
We prioritize patient comfort and satisfaction, creating a supportive environment for optimal healing.
Post-Treatment Support
Our robust post-treatment support ensures ongoing patient care through recovery and rehabilitation services.