Learn about the conditions and
treatments we specialize in at
Modern Orthopaedics of NJ.
Top Orthopaedic Care in NJ
At Modern Orthopaedics of New Jersey, we offer top Orthopaedic care in Wayne, Parsippany and Paramus.

Shoulder
Conditions & Procedures
Rotator Cuff
Rotator Cuff Tear Treatment and Surgery in Wayne, Paramus, and Parsippany NJ
Many sports involve repetitive arm motions that can take a toll on the rotator cuff tendons that surround the shoulder. The shoulder is a ball and socket joint that is composed of the humerus bone in the upper arm, the scapula, and the clavicle. The shoulder joint is surrounded by four tendons that make up the rotator cuff. These tendons attach to muscles that are in charge of lifting and rotating your arm. The four tendons are the supraspinatus, infraspinatus, subscapularis, and teres minor. Any of these tendons can be involved in a rotator cuff injury.
Arthritis, Arthroscopy & Replacement
Shoulder Arthritis, Arthroscopy & Replacement in Wayne, Paramus, and Parsippany NJ
Shoulder or glenohumeral arthritis occurs over time as joint cartilage is worn down and destroyed, narrowing the joint space. This can be the result of degenerative changes, posttraumatic arthritis or inflammatory arthritis. Patients describe the pain as being worse with any kind of movement or strenuous activity and therefore motion tends to be limited. X-rays will reveal narrowed or negligent remaining joint space between the humeral head and the glenoid. Initial treatment usually consists of rest, NSAIDs, therapy and cortisone injections. Ultimately, depending on the patient’s health and age, a total shoulder arthroplasty may be indicated to alleviate pain and restore some function. If the rotator cuff is also compromised, a reverse total shoulder arthroplasty may be necessary.
Frozen Shoulder
Frozen Shoulder Treatment and Surgery in Wayne, Paramus, and Parsippany NJ
Adhesive Capsulitis (Frozen Shoulder)
Frozen shoulder, also known as adhesive capsulitis, most commonly affects patients between the ages of 40 to 60. It results in a loss of both active and passive range of motion and can be quite painful. It is more common in women and in patients with diabetes. The most common presenting symptoms are pain and loss of range of motion. It is not usually associated with trauma but may develop after a period of shoulder immobilization or surgery. Imaging is usually not necessary, but an MRI may show a contracted capsule and loss of the inferior pouch. Conservative treatment usually consists of a cortisone injection and extensive formal physical therapy to regain range of motion. Participation in a rigorous therapy program is crucial in the recovery of frozen shoulder. Patients should notice a significant improvement in pain and function within the first six to eight weeks of therapy. In rare cases, surgical intervention may be warranted for an arthroscopic capsular release and lysis of adhesions.
Clavicle Fracture
Clavicle Fracture Treatment and Surgery in Wayne, Paramus, and Parsippany NJ
The clavicle, also known as the collar bone, is an S-shaped bone that connects to the sternum.
Clavicle Fracture (Collar Bone Fracture)
The clavicle is an S-shaped bone that connects to the sternum medially and to the scapula laterally. A clavicle fracture can occur from direct trauma or falling onto the shoulder or arm. It is not uncommon to see clavicle fractures in cyclists, snowboarders, or football players who have fallen onto the shoulder. The fracture can occur anywhere along the length of the bone although it most commonly occurs in the middle portion of the bone.
Most athletes that have suffered a clavicle fracture will present with pain over the clavicle and a history of trauma. There may be tenting or pushing up of the skin over the fracture site. The clavicle bone site close to the skin surface and a displaced fracture or sharp fracture edge may threaten the skin. Our doctors will carefully examine your shoulder and clavicle area and order x-rays. Plain x-rays are used to evaluate the clavicle fracture and assess the fracture pattern, displacement, angulation, comminution, and shortening. After the fracture is assessed, appropriate management is decided upon by your orthopedic doctor. Generally, further imaging is not necessary unless your doctor suspects any tendon or ligament damage related to the injury.
Traditionally, clavicle fractures were managed conservatively in the pediatric, adolescent, and adult population, but more recent studies have shown that operative intervention may allow patients to return to activities more quickly, have quicker radiographic union, less chance of nonunion or malunion, and less pain during recovery. Clavicle malunion is usually a result of clavicle shortening and displacement. A malunion can potentially alter the kinematics of the scapula, leading to scapular dyskinesis and malrotation. Studies have shown that clavicular malunion in skeletally mature patients causes decrease in strength and velocity with certain movements of the upper arm, and it is thought that this may be true in adolescent patients as well.
Typically, pediatric clavicle fractures with little displacement and minimal shortening can be treated without surgery. Treatment generally consists of immobilizing the arm in a sling for 4 weeks. After that point the patient can begin range of motion and will generally be ready to return to activities 8-12 weeks after the fracture.
Surgical management of midshaft clavicle fractures is usually warranted when there is >15mm of significant shortening, 100% displacement, or significant comminution especially in pediatric patients involved in high demand activities. It has been shown that in pediatric patients 10 years and older with these fracture patterns use of an elastic stable intramedullary nail leads to less pain during recovery, increased patient satisfaction, and less time immobilized.
There are two options to consider when surgical management is decided. The first is fixing the bone with a plate and screws that lie on top of the bone. This will provide a secure and adequate reduction, although it does require stripping of muscle off the bone where the plate will rest.
The plate and screws also require an extensive incision over a good portion of the clavicle so it can be positioned properly. The patient may be able to feel the plate after surgery and it can potentially be bothersome when wearing a backpack, purse, or anything that puts pressure on the collarbone. A clavicle plate may oftentimes need to be removed with a second surgery due to the irritation it causes. Despite the drawbacks of using a clavicle plate and screws it may be the best option if the fracture is significantly comminuted or in multiple pieces.
Clavicle Fracture (Collar Bone Fracture)
The second option is fixing the bone with a clavicle nail. Although, this is a good option it is not appropriate for every fracture. A clavicle nail sits inside the bone in the intramedullary canal.
This eliminates the need to strip down muscle overlying the clavicle. The surgery is done through three small incisions. The hardware is placed inside the bone and cannot be felt by the patient after surgery. The clavicle nail also eliminates the irritation that patients sometimes experience from straps and backpacks. Rarely is this hardware removed after surgery. Our doctors will closely monitor your progress and healing with x-rays after surgery. Physical therapy may be part of your rehabilitation to help regain your motion and strength. Your doctor will let you know when it is safe to return to play and at what point you are released to use the hand without restrictions.
A clavicle fracture can cause serious setbacks for any athlete. Our goal at Modern Orthopaedics is for you to return to your sport better than before. This may take time and patience, but we want you to experience a full recovery. We understand that each athlete and sport is unique and we will develop your treatment plans accordingly. We want to understand your goals and help you reach them. Please contact our office to have an initial evaluation for a shoulder or clavicle injury and receive superior care from our doctors and staff.

Labral Tear
Labral Tear Treatment and Surgery in Wayne, Paramus, and Parsippany NJ
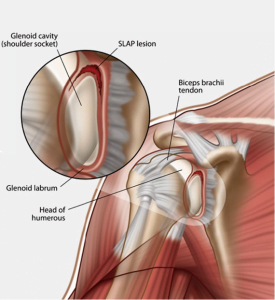
Labral tears of the shoulder involve the cartilaginous lining of the glenoid (socket).
The shoulder is a ball and socket joint that is composed of the humerus bone in the upper arm, the scapula, and the clavicle. The head or “ball” of the humerus sits in the socket portion of the scapula called the glenoid. The cartilaginous lining around the outside of the glenoid is called the labrum. The labrum helps to stabilize the shoulder and deepen the socket, or the glenoid. The labrum essentially functions as a bumper that helps stabilize the shoulder. Athletes that sustain a shoulder subluxation or dislocation may concurrently injure their labrum. In these cases, the labrum is torn off the bone when the humeral head comes out of the socket. This tear may also make the shoulder less stable and increase the shoulder’s propensity to sublux or dislocate again. Many times an athlete may not even realize that their shoulder is sliding in and out of the socket, but they have shoulder pain and sometimes catching or clicking.
Other labral injuries involve the biceps tendon which attaches to the top or superior portion of the labrum. These are often referred to as SLAP tears, superior labral tear from anterior to posterior, and are a common type of labral tear. This injury is common in athletes when exerting maximum effort throwing, but is also seen in patients who may experience pain with overhead activities. There are different types of SLAP tears and they are classified according to the severity of the tear and the involvement of the biceps tendon. These athletes usually present with pain and sometimes catching or clicking in the shoulder with certain motions. Athletes affected by labral tears are likely unable to achieve peak performance due to pain. Sports that require extensive arm and overhead motion may be near impossible to play in some cases.
SLAP tears are a common overuse injury in baseball and softball players. It is important for athletes, coaches, and parents to understand the importance of limiting pitch count, especially in young athletes. Proper technique is also extremely important and can help to avoid unnecessary injury to the shoulder. Lastly, stretching and strength training is crucial for any athlete. If you or your coaches are unsure as to what stretches, exercises, or muscle groups to focus on don’t hesitate to reach out to a local physical therapist who can help.
Labral tears are sometimes difficult to diagnose with physical examination alone. An MRI and an MR arthrogram is a good diagnostic test used to evaluate for labral tears. Although not always necessary, a MR arthrogram may be done where dye is injected into the shoulder joint. This dye allows your doctor to more clearly visualize labral tears in particular. If for some reason a labral tear cannot be visualized on an MRI, but is still highly suspected then a shoulder arthroscopy is the best way to definitively diagnose the problem. A shoulder arthroscopy is invasive, but will allow your doctor to directly see the labrum and surrounding structures.
Initial treatment for small labral tears or fraying may be conservative and involve anti-inflammatory medications and rehabilitation focused on strengthening of the rotator cuff muscles and periscapular stabilization. Physical therapy can often strengthen the surrounding muscles and alleviate or eliminate the pain. Usually if physical therapy is prescribed, our doctors will recommend that you stick with it for at least 6 weeks to see if it actually makes an improvement. Oftentimes, patients are surprised by the improvement they have with physical therapy and they can return to their sport stronger than before. Other patients do not have success with conservative management and they may be a candidate for an arthroscopic labral repair.
Labral repairs are done arthroscopically. Shoulder arthroscopy involves introducing a small camera and instruments into the shoulder joint through a series of small incisions to examine different parts of the shoulder. This may oftentimes be both diagnostic and therapeutic. Arthroscopy allows your surgeon to visualize the labrum, biceps tendon, capsular ligaments, undersurface and superior surface of the rotator cuff, the glenoid, humeral head, and subacromial space. Debridement and repair of the labrum can be done through the small portals made in the shoulder.
Labral Tear
The repair involves putting the labral tissue back in its native location around the glenoid. Anchors are placed in the bone, and sutures are used to secure the labrum. Your surgeon will also clean up any frayed tissues and address any other issues in the shoulder. The biceps tendon may be repaired, but often the biceps tendon is cut and attached in a different location or just left alone. Your surgeon will discuss these treatment options with you prior to your surgery.
Rehabilitation following a labral repair is very important. Early gentle motion is encouraged after surgery to avoid stiffness. Your therapist will guide you through specific motions and exercises that are prescribed by your doctor. At about two months after surgery, the patient can begin to progress their physical therapy to stretching and strengthening exercises. A full recovery can be expected within three to six months after surgery.
Labral tears can cause serious setbacks for any athlete. Our goal at Modern Orthopaedics is for you to return to your sport better than before. This may take time and patience, but we want you to experience a full recovery. We understand that each athlete and sport is unique and we will develop your treatment plans accordingly. We want to understand your goals and help you reach them. Please contact our office to have an initial evaluation for shoulder pain and receive superior care from our doctors and staff.
Proximal Humerus Fracture
Proximal Humerus Fracture Treatment and Surgery in Wayne, Paramus, and Parsippany NJ
Proximal humerus fractures can occur in many different fracture patterns involving the greater tuberosity, lesser tuberosity, surgical neck or may be associated with a dislocation. Many of these fractures may be treated with nonoperative management, but others need to be treated surgically taking into consideration the age and health of the patient. If treated nonoperatively, the patient will rest the arm in a sling for four to six weeks. They generally begin to do pendulum exercises about three weeks after the fracture and begin range of motion with the shoulder at about four weeks. This will be determined at follow up appointments after careful examination and x-rays to check the alignment and healing of the fracture.
Generally, we try to get the shoulder moving again as soon as possible to avoid frozen shoulder. The patient will likely return to their normal activities after the fracture heals, although in some cases they may have decreased range of motion when compared with the uninjured side.

Shoulder Instability
Shoulder Instability Treatment and Surgery in Wayne, Paramus, and Parsippany NJ
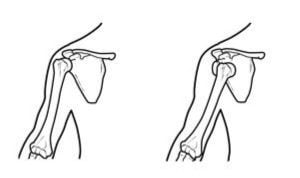
The shoulder joint has exceptional mobility and is the most commonly dislocated large joint.
The shoulder joint has exceptional mobility and is the most commonly dislocated large joint. Males aged 10 to 20 years old are the most common first time dislocators, followed by those in the 50 to 60 year age group. Often times shoulder subluxation or dislocation may be recurrent, as once the shoulder has initially dislocated, it is more prone to do so again in the future. The shoulder may be unstable anteriorly, posteriorly, inferiorly or multidirectionally. Initial traumatic dislocations are most likely the result of a fall, trauma or forceful throwing motion. Shoulder dislocations are also much less commonly atraumatic are caused by ligamentous laxity, connective tissue disease or bony abnormalities.
The shoulder is usually put back in place (reduced) in the emergency room. Unfortunately, many times there may be associated injuries that the patient is unaware of. Studies have shown that one in every three patients will sustain a greater tuberosity fracture or a rotator cuff tear after a primary shoulder dislocation. In patients over the age of 40, the likelihood of having an associated rotator cuff tear increases dramatically. Associated labral tears and axillary nerve traction injuries are also not uncommon. Children who have not reached skeletal maturity are more likely to sustain injuries to their growth plates. The elasticity of the shoulder capsule in young children may help prevent damage to the capsulolabral complex and decrease the likelihood of redislocation. It is important that patients of all ages follow up in an orthopedic office after shoulder dislocations for further evaluation. Associated injuries are oftentimes overlooked if not evaluated by a specialist.
After an acute dislocation is reduced the patient will likely be immobilized in a sling for three to four weeks. Often times an MRI will be obtained if there is suspicion of an associated rotator cuff tear or labral pathology. CT scans may be ordered if there is suspected bone loss or fracture. Redislocation is most common in males under the age of 20 but may occur in older patients as well. Instability may be the result of soft tissue or a bony deficiency. In the case of recurrent dislocation, surgery may be necessary. A Bankart lesion is a tear of the labrum and detachment of the inferior glenohumeral ligament that results from an anterior-inferior dislocation of the humerus. Hill-Sachs lesions, impression fractures in the humeral head, often result from glenohumeral dislocations. The glenoid itself, the socket part of the joint, may also be fractured as a result of dislocation making it difficult to ensure stability by only addressing the soft tissues. In this case, a Latarjet procedure may be necessary, which involves transferring autograft from the distal coracoid into the glenoid defect.
Throwing Shoulder
Throwing Shoulder Treatment and Surgery in Wayne, Paramus, and Parsippany NJ
Shoulder injuries are very common in the throwing athlete.
Shoulder injuries are very common in the throwing athlete. The use of high-speed video technology has shown that pitching a baseball requires the arm to accelerate at a speed of 7,000 degrees per second. Larger muscles surrounding the shoulder are most active during the acceleration of the throw, whereas the smaller, more delicate rotator cuff muscles are most active during the deceleration phase.
Our specialists will evaluate the throwing athlete by obtaining a thorough history and physical exam. A series of tests will be performed on both shoulders to compare range of motion, strength and evaluate maneuvers that elicit pain. Radiographic imaging and MRIs will be obtained when necessary for diagnosing the problem. Microtrauma injuries to the rotator cuff muscles are common and can cause pain while throwing, whereas more significant tears may cause profuse night pain. Instability may cause pain or give the sensation of subluxation especially during the follow through phase of throwing. Athletes that are experiencing decreased range of motion, particularly internal rotation, may have contracture of the posterior capsule.
Treatment for shoulder injuries in the throwing athlete will be focused on the patient’s specific issue. There are many different possible pathologies in the shoulder that can cause pain and dysfunction. Our shoulder specialists focus on conservative management initially which usually requires physical therapy directed toward strengthening the shoulder girdle, stretching and decreasing pain. If there are no improvements seen over a three to six month time period, surgical treatment may be considered.

Shoulder Arthroscopy
Shoulder Arthroscopy in Wayne, Paramus, and Parsippany NJ
Shoulder arthroscopy is a surgical procedure done with a small camera and instruments through small incisions called portals.
Shoulder arthroscopy involves introducing a small camera and instruments into the shoulder joint through a series of small incisions to examine different parts of the shoulder. This may oftentimes be both therapeutic and diagnostic. Arthroscopy allows the surgeon to visualize the labrum, biceps tendon, capsular ligaments, undersurface and superior surface of the rotator cuff, the glenoid, humeral head and subacromial space. Debridement and repair of injured structures can be done when necessary through the small portals made in the shoulder. The overall goal is to restore normal function and stability while eliminating pain and avoiding large surgical incisions.
Clavicle ORIF
Clavicle ORIF (Open Reduction and Internal Fixation) in Wayne, Paramus, and Parsippany NJ
Hardware is used to correct significantly displaced or comminuted clavicle fractures.
Surgical management of midshaft clavicle fractures is usually warranted when there is >15mm of significant shortening, 100 percent displacement, or significant comminution, especially in pediatric patients involved in high-demand activities. It has been shown that in pediatric patients 10 years and older with these fracture patterns, the use of an elastic stable intramedullary nail leads to less pain during recovery, increased patient satisfaction, and less time immobilized.
There are two options to consider when surgical management is decided. The first is fixing the bone with a plate and screws that lie on top of the bone. This will provide a secure and adequate reduction, although it does require stripping of muscle off the bone where the plate will rest. The plate and screws also require an extensive incision over the majority of the clavicle so it can be positioned properly. The patient may be able to feel the plate after surgery and it can potentially be bothersome when wearing a backpack, purse, or anything that puts pressure on the collarbone. A clavicle plate often needs to be removed with a second surgery due to the irritation it causes. Despite the drawbacks of using a clavicle plate and screws, it may be the best option if the fracture is significantly comminuted or in multiple pieces.
The second option is fixing the bone with a clavicle nail. A clavicle nail sits inside the bone in the intramedullary canal. This eliminates the need to strip down muscle overlying the clavicle. The surgery is done through three small incisions. The hardware is placed inside the bone and cannot be felt by the patient after surgery. The clavicle nail also eliminates the irritation that patients sometimes experience from straps and backpacks. The clavicle nail rarely needs to be removed after surgery.
Clavicle ORIF (Open Reduction and Internal Fixation)
Clavicle ORIF (Open Reduction and Internal Fixation)
The second option is fixing the bone with a clavicle nail. A clavicle nail sits inside the bone in the intramedullary canal. This eliminates the need to strip down muscle overlying the clavicle. The surgery is done through three small incisions. The hardware is placed inside the bone and cannot be felt by the patient after surgery. The clavicle nail also eliminates the irritation that patients sometimes experience from straps and backpacks. The clavicle nail rarely needs to be removed after surgery.
Arthroscopic Labral Repair of the Shoulder
Arthroscopic Labral Repair of the Shoulder in Wayne, Paramus, and Parsippany NJ
Labral repairs involve repairing the labrum back to its native location around the glenoid.
Labral repairs involve repairing the labrum back to its native location around the glenoid. Anchors are placed in the bone, and sutures are used to secure the labrum. Early gentle motion is encouraged about two weeks after surgery to avoid stiffness. At about two months post-op, the patient can begin to progress their physical therapy to stretching and strengthening exercises. A full recovery can be expected within three to six months after surgery.
Arthroscopic Lysis of Adhesions
Arthroscopic Lysis of Adhesions in Wayne, Paramus, and Parsippany NJ
Arthroscopic surgery performed for persistent frozen shoulder.
If a frozen shoulder persists despite cortisone injections and therapy, the patient may be a candidate for arthroscopic lysis of adhesions. The shoulder arthroscopy is a surgical procedure done with a small camera and instruments through small incisions called portals. This procedure allows the surgeon to directly visualize and release the adhesions that are restricting motion. The shoulder will also be manipulated in the operating room to measure the motion after the capsular release. Physical therapy will be a crucial part of the postoperative recovery and will begin almost immediately after surgery to ensure that the patient retains the motion gained in the operating room. The patient’s progress will be carefully monitored by their surgeon and physical therapists. Once the patient’s motion has improved, it is critical that they continue to do the exercises on their own to avoid developing the problem again in the future.
Arthroscopic Rotator Cuff Repair
Arthroscopic Rotator Cuff Repair in Wayne & Paramus, NJ
Arthroscopic procedure to treat rotator cuff injuries and tears.
Shoulder arthroscopy involves introducing a small camera and instruments into the shoulder joint through a series of small incisions to examine different parts of the shoulder. This may oftentimes be both therapeutic and diagnostic. Arthroscopy allows the surgeon to visualize the labrum, biceps tendon, capsular ligaments, undersurface and superior surface of the rotator cuff, the glenoid, humeral head, and subacromial space. Debridement and repair of injured structures can be done when necessary through the small portals made in the shoulder. The overall goal is to restore normal function and stability while eliminating pain.
Rotator cuff repairs involve returning the torn tendon to its native location with the use of anchors placed in the bone and sutures drawn through the torn end of the tendon. For the first six weeks after surgery, you will have to rest your shoulder in a sling with very limited shoulder motion. The tendon will take about six weeks to heal down to the bone. Once the six weeks has passed, the patient may begin gentle range of motion exercises with formal physical but must wait three months before it is safe to do any kind of resistance or strengthening exercises. The entire recovery process takes anywhere from six months to one year after surgery.
Proximal Humerus ORIF
Proximal Humerus ORIF (Open Reduction Internal Fixation) in Wayne, Paramus, and Parsippany NJ
Surgical fixation of humerus fractures near the shoulder.
Surgical intervention may be necessary with a proximal humerus fracture depending on the type of fracture and degree of displacement. In patients with a greater tuberosity fracture with displacement, surgery may be required to restore normal function to the rotator cuff muscles. In other cases, a hemiarthroplasty may be required if the blood supply to the humeral head has been disrupted. Sometimes the fracture can be fixed with a plate and screws used to realign the fracture and keep it in anatomic alignment while it heals. Regardless of the technique used for treatment, each patient will be closely followed after their surgery to ensure proper healing and maintained alignment.
Shoulder Arthroplasty
Shoulder Arthroplasty in in Wayne, Paramus, and Parsippany NJ
Procedure for patients with advanced shoulder arthritis.
Total Shoulder Arthroplasty
Some patients with advanced shoulder arthritis and an intact rotator cuff may be a candidate for a total shoulder arthroplasty (aka total shoulder replacement). It is important to take into consideration the patient’s age and functional status when considering this option. The total shoulder replacement will help decrease pain and allow the patient to return to daily activities. It is generally not designed for heavy laborers or those involved in daily strenuous activities. The surgery involves replacing two components from within the shoulder: the humeral head (ball) and the glenoid (socket). The patient will begin gentle range of motion shortly after surgery. The patient’s progress will be followed closely by their surgeon and physical therapist at follow-up appointments.
Reverse Total Shoulder Arthroplasty
This surgery is reserved for patients with advanced shoulder arthritis in combination with a torn and retracted rotator cuff. The reverse shoulder arthroplasty changes the dynamics of the shoulder so that the deltoid muscle takes the place of the rotator cuff when elevating the arm. The native humeral head is replaced with the socket portion of the arthroplasty, and the glenoid is replaced with the ball portion of the arthroplasty. Shoulder range of motion will likely still be limited after surgery, but pain will be relieved once the arthritic joint is replaced.
Elbow
Conditions & Procedures
Cubital Tunnel Syndrome
Cubital Tunnel Syndrome Treatment and Surgery in Wayne & Paramus, NJ
Cubital tunnel syndrome is a common condition that involves compression of the ulnar nerve at the elbow. The nerve is compressed in a groove along the posterior aspect of the medial epicondyle. This syndrome can develop acutely after direct trauma or chronically over time. Symptoms usually involve aching pain over the medial aspect (inside) of the elbow and numbness and tingling in the ring and small fingers. Prolonged compression may result in weakness and muscle wasting in more severe cases. A thorough clinical examination, along with nerve conduction studies, will help confirm the diagnosis of cubital tunnel syndrome. Initial treatment usually involves activity modification, night splinting and NSAIDs in more acute cases. If conservative management fails, surgical decompression and transposition of the ulnar nerve may be considered.
Cubital Tunnel Release and Ulnar Nerve Transposition
Cubital Tunnel Release and Ulnar Nerve Transposition in Wayne & Paramus, NJ
A surgical release of the ulnar nerve within the cubital tunnel.
A cubital tunnel release with or without ulnar nerve transposition is the surgical treatment for cubital tunnel syndrome. This may be considered if a patient has persistent symptoms and dysfunction despite conservative management. The patient’s symptoms of numbness, tingling and sometimes weakness are a result of excess pressure on the ulnar nerve. The surgery involves decompressing the ulnar nerve from a tight tunnel of tissue that is putting pressure on the nerve. Sometimes an ulnar nerve transposition may also be done to move the nerve into a less vulnerable position. The surgery involves an incision over the inside of the elbow. The patient is generally placed in a soft dressing after surgery and recovery is usually two to three weeks to allow the incision to fully heal. At this point, you can return to activities as tolerated. If the nerve compression was severe, the recovery of sensation may take several months to a year.
Distal Humerus Fracture
Distal Humerus Fracture Treatment and Surgery in Wayne & Paramus, NJ
Fracture of the humerus bone down near the elbow.
There are many different types of fractures that can occur in and around the elbow joint. The severity and location of the fracture will determine the course of treatment. Distal humerus fractures account for about 2 percent of all fractures in adults. They present with pain and swelling in and around the elbow joint. Definitive diagnosis is made with x-rays. Sometimes a CT scan may be done for a more detailed picture of the fracture. Treatment depends on the level of displacement, fracture location and involvement of neurovascular structures. Stable nondisplaced fractures may be treated with splinting, but more commonly distal humerus fractures are displaced and require open reduction and internal fixation.

Distal Humerus ORIF
Distal Humerus ORIF in Wayne & Paramus, NJ
Surgical fixation of humerus fractures near the elbow with plates and screws.
Distal Humerus ORIF (Open Reduction Internal Fixation)
Distal humerus fractures often have to be treated surgically with plates and screws that are fixated to the bone to stabilize the fracture. Depending on the location and type of fracture, more than one plate may be used on either side of the bone. Early guided range of motion may be encouraged to prevent stiffness. X-rays will be taken at follow-up appointments to ensure proper healing and maintained alignment. The bone will usually take four to six weeks to heal, but the rehab process will take several months.
Elbow Contracture
Elbow Contracture Treatment and Surgery in Wayne & Paramus, NJ
Elbow contractures restrict your elbow motion and may be painful.
An elbow contracture can develop as result of a previous trauma, surgery or a systemic inflammatory condition. The contracture will restrict your elbow motion and may be painful. The contracture may be due to a bony abnormality preventing the joint from normal function or from the surrounding soft tissues. If the issue is due to soft tissue, initial treatment may involve therapy, serial splinting and cortisone injections. If the issue involves bony abnormalities, or conservative management with soft tissue contracture has failed, surgical intervention may be necessary. Radiographs, CT or MRI may be necessary imaging tools used to determine the extent of involvement in the joint and soft tissues.

Elbow Contracture Release
Elbow Contracture Release in Wayne & Paramus, NJ
Surgical removal of soft tissue or loose bodies that block motion and cause pain at the elbow.
When an elbow contracture cannot be treated conservatively, surgical management may be indicated for a patient to regain motion and function of the elbow. This can be done through an open or arthroscopic approach. In either case, it involves removing soft tissue, synovitis and possibly loose bony fragments that may be blocking motion and causing pain. Physical therapy and bracing are a crucial part of the recovery process and generally begin immediately after surgery to retain the motion that was gained from the surgery.
Elbow Dislocation
Elbow Dislocation Treatment and Surgery in Wayne & Paramus, NJ
Elbow dislocation is injury to the elbow where the joint is disrupted.
Elbow dislocations commonly occur in both children and adults. They usually occur as a result of a fall onto an outstretched hand. The elbow can dislocate in all directions, although most commonly it is posterolateral. The lateral and medial collateral ligaments are commonly disrupted as a result of elbow dislocations. Radial head and coronoid process fractures may also be associated with this injury. This injury may be treated with closed reduction and splinting, although if the reduction is unstable or has concomitant issues, it may need to be treated surgically. Please refer to our “Treatments” section for more information.

Open Elbow Reduction
Open Elbow Reduction in Wayne & Paramus, NJ
An open surgical reduction of elbow dislocations.
An open elbow reduction is usually reserved for an elbow dislocation that may be complicated by concomitant fractures or unstable reduction. Extensive soft tissue and ligamentous injury may also need to be addressed during surgery as well as any bony loose bodies or fractures. Generally, motion will begin within a few days after surgery with a therapist and a specific protocol to avoid stiffness.
Tennis Elbow
Tennis Elbow Treatment and Surgery in Wayne & Paramus, NJ
Lateral epicondylitis, commonly known as tennis elbow, is a condition of the elbow that often causes pain on the outside of the elbow with lifting, gripping and activities that involve wrist extension.
The humerus of the upper arm and the radius and ulna of the forearm meet to form the elbow joint. The elbow is surrounded by many different ligaments, vessels, nerves, muscles, and tendons. One tendon in particular contributes to the pain experienced by a patient with tennis elbow. This tendon originates on the outside of the elbow on the lateral epicondyle and turns into the extensor carpi radialis brevis muscle. This muscle is in charge of wrist extension. When this tendon experiences a significant amount of force and repetitive strain it can develop microtears that lead to tennis elbow. Tennis players may be predisposed to developing this condition, but it is common in many different athletes. It is also common among patients who have occupations that involve repetitive motion of the wrist and elbow, such as painters and plumbers.
Golfer’s Elbow - Medial Epicondylitis
Golfer’s Elbow – Medial Epicondylitis Treatment and Surgery in Wayne & Paramus, NJ
The humerus of the upper arm and the radius and ulna of the forearm meet to form the elbow joint. The elbow is surrounded by many different ligaments, vessels, nerves, muscles, and tendons. Several tendons can contribute to the pain experienced by a patient with golfer’s elbow. These tendons originate on the inside of the elbow on the medial epicondyle and are in charge of flexing the fingers and turning the palm up. When these tendons experience a significant amount of force and repetitive strain they can develop microtears that lead to golfer’s elbow. Golfer’s may be predisposed to developing this condition, but it is very common in many climbing athletes and baseball players as well.
Olecranon Fractures
Olecranon Fractures Treatment and Surgery in Wayne & Paramus, NJ
Olecranon fractures are fractures of the bony prominence that most associate with the elbow.
Olecranon fractures are fractures of the bony prominence that most associate with the elbow. These fractures may be the result of a direct blow to the olecranon or associated with elbow dislocations. Nondisplaced fractures may be treated with splinting and a sling. The fracture will take four to six weeks to heal, and physical therapy will likely be a part of the rehabilitation process once the fracture has healed. Displaced or more complex fractures are usually indicated for surgery, and early range of motion is encouraged to avoid stiffness.

Olecranon ORIF
Olecranon ORIF in Wayne & Paramus, NJ
An incision is made directly over the fracture, and the bones are placed back into anatomic alignment and secured with a plate and screws or a tension band wire construct.
Olecranon ORIF (Open Reduction Internal Fixation)
Surgical intervention may be necessary to ensure healing and return to function following an olecranon elbow fracture. This is usually a same-day procedure that is done at a hospital or surgery center. An incision is made directly over the fracture, and the bones are placed back into anatomic alignment and secured with a plate and screws or a tension band wire construct. It will take four to six weeks for the fracture itself to heal, but early elbow range of motion will be encouraged to prevent stiffness. Physical therapy will likely be a part of the rehabilitation process to help regain motion and strength.
Radial Head Fracture
Radial Head Fracture Treatment and Surgery in Wayne & Paramus, NJ
Radial head fractures are fractures of the radius at the elbow.
Radial head and neck fractures usually result from a fall on an outstretched hand. These fractures are classified into three types according to the Mason classification: Type I fractures are nondisplaced, Type II fractures are displaced greater than 2mm at the articular surface or angulated neck fractures and Type III fractures are severely comminuted fractures of the head and neck. Type I fractures are usually treated conservatively with splinting and early range of motion as tolerated. Type II and III fractures are usually treated with open reduction and internal fixation. On occasion with severe comminution, a radial head replacement may be indicated.

Radial Tunnel Release
Radial Tunnel Release in Wayne & Paramus, NJ
This surgery involves an incision over the dorsal forearm and dissection down to the level of nerve compression.
A radial tunnel release is done when symptoms persist despite conservative management. This surgery involves an incision over the dorsal forearm and dissection down to the level of nerve compression. The supinator muscle and other structures overlying the nerve are incised and the posterior interosseous nerve is decompressed. This should give the patient relief of their symptoms, and they will regain normal function of their arm in two to three weeks once the incision has fully healed.
Radial Head Arthroplasty
Radial Head Arthroplasty in Wayne & Paramus, NJ
Replacement of the radial head with prosthetic hardware.
A radial head arthroplasty is done when a radial head fracture is comminuted and therefore an open reduction and internal fixation (ORIF) is not possible. Many times, this type of fracture is associated with an elbow dislocation. The surgery involves removing the radial head and portion of the radial neck and replacing it with a prosthetic radial head. Postoperative recovery will involve therapy to regain motion and strength. Generally, physical therapy begins shortly after surgery.
Radial Tunnel Syndrome
Radial Tunnel Syndrome Treatment and Surgery in Wayne & Paramus, NJ
Radial tunnel syndrome develops from compression of a branch of the radial nerve called the posterior interosseous nerve in the forearm.
Radial tunnel syndrome develops from compression of a branch of the radial nerve called the posterior interosseous nerve in the forearm, as it runs between muscle bellies and under fascial bands. Patients may describe this as a burning and aching pain in the forearm. It is usually not associated with injury, although it is possible. Diagnosis is often done clinically, as nerve tests and MRIs are usually not helpful. Initial treatment may involve rest and anti-inflammatories, but if these conservative measures fail, surgical intervention may be indicated.

Pediatric Elbow Fracture
Pediatric Elbow Fracture Treatment and Surgery in Wayne & Paramus, NJ
If your child sustains a fall and experiences difficulty moving their elbow, swelling to the area or the arm appears crooked, you should seek immediate medical attention.
Pediatric elbow fractures make up about 10 percent of all pediatric fractures and come in a variety of shapes and sizes. There are three bones that make up the elbow joint allowing you to bend and straighten your arm and turn your palm up and down. If your child sustains a fall and experiences difficulty moving their elbow, swelling to the area or the arm appears crooked, you should seek immediate medical attention. Some fractures around the elbow can be treated with a cast only while others require surgery. It is not uncommon for kids to have occult (or hidden) fractures around the elbow that show up only as swelling on an x-ray. In this case, the physician may recommend placing the child in a cast for several weeks until evidence of healing can be seen on another x-ray. In some cases, if the fracture is displaced, then surgical intervention may be indicated. See our “Elbow Surgery” section for more information.

Supracondylar/Condylar CRPP
Supracondylar/Condylar CRPP in Wayne & Paramus, NJ\
Elbow fractures treated with wires and screws in addition to a cast.
Supracondylar/Condylar CRPP (Closed Reduction Percutaneous Pinning)
If a pediatric elbow fracture is displaced, surgery may be recommended to realign the bone and hold it in place with wires or screws in addition to a cast. The patient would then be followed closely in the office with serial x-rays to ensure bone alignment is maintained. Wires that are used to help realign the bone are typically removed in the office several weeks after surgery. If screws are utilized, sometimes these will need to be removed several months later with an additional surgery to allow for continued bone growth. Children generally regain their motion and strength without therapy, but in some cases physical therapy may be utilized.
Extensor Carpi Radialis Brevis Debridement (PRP Injection)
Extensor Carpi Radialis Brevis Debridement (PRP Injection) in Wayne & Paramus, NJ
Platelet-rich plasma or PRP injections involve injecting the patient’s own platelets at a high concentration into the site of the tendon injury to promote further healing.
PRP injection
Some patients have persistent lateral epicondylitis (tennis elbow) despite conservative management. In these cases, further treatment is indicated. Platelet-rich plasma or PRP injections involve injecting the patient’s own platelets at a high concentration into the site of the tendon injury to promote further healing. This treatment may be a good initial option prior to pursuing a more invasive surgical intervention. PRP injections are less invasive and can be done in the office. It is important to keep in mind that it may take several rounds of injections for patients to notice an improvement in their symptoms.
Extensor carpi radialis brevis debridement
When other treatment options are unsuccessful, surgical intervention is indicated. This usually involves debridement of the contributing ECRB tendon. The tendon debridement may be done with a small incision directly over the area or arthroscopically with a camera introduced into the elbow joint. In either case, the ECRB tendon is identified and debrided (devitalized or frayed tissue is removed) to promote healing and decrease pain. The patient is usually placed in a soft dressing postoperatively and begins elbow range of motion right away. The patient is usually able to return to most activities within three to four weeks.
Hand & Wrist
Conditions & Procedures
Phalanx (Finger) Fractures
Phalanx Fracture Treatment in Wayne, Paramus, and Parsippany NJ
Phalanx fractures are fractures of the small bones that make up the fingers.
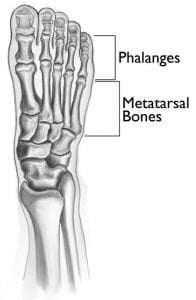
Phalanges are the small bones that make up the fingers. Each finger has a distal, middle and proximal phalanx, and the thumb has a distal and proximal phalanx. Phalangeal fractures in adults most commonly involve the distal phalanx, while in children injuries to the growth plate of the small finger are most common. Regardless of the patient’s age or location of pain, this diagnosis is made by examination and x-rays. Treatment of theses fractures depends on the bone involved and the type of fracture. Attention must also be given to the rotation of the fingers that may be associated with a phalangeal fracture. There are a variety of fracture patterns, and each one calls for treatment tailored to that specific type of fracture. Some fractures can be immobilized in a cast or splint, other fractures may need to be manipulated into proper alignment and some may require surgical intervention for reduction and fixation of the fracture.

Phalanx (Finger) CRPP and Phalanx ORIF
Phalanx CRPP and Phalanx ORIF Treatment in Wayne, Paramus, and Parsippany NJ
Metacarpal (Hand) Fracture
Metacarpal Fracture Treatment in Wayne, Paramus, and Parsippany NJ
Metacarpal fractures are common fractures in the hand that usually occur when a closed fist strikes an object.
The hand consists of many small bones, muscles, and tendons that articulate and work together to allow for fine motor movements, dexterity, and strength. The metacarpals are the long bones in the hand that connect to the fingers. The head of the metacarpal bones are what makes the prominence of your knuckles when you make a fist. Metacarpal fractures commonly occur during motor vehicle accidents, falls, or other trauma.
Metacarpal fractures can affect patients of all ages. Unfortunately, they affect use of the hand for grasping, lifting, catching, throwing, or balance. Generally, there will be swelling and pain over the top of the hand. There will also be a history of trauma and you may have difficulty making a fist. Sometimes your involved knuckle may appear less prominent than usual. If you are experiencing any of these symptoms you should be evaluated by one of our doctors.
At your initial evaluation, our doctors will carefully examine your hand and take x-rays to confirm your diagnosis. Your treatment will depend on the severity of your fracture and a variety of other factors. Fractures that are non-displaced or minimally displaced can be treated conservatively in a cast or a splint. These fractures will generally heal in about 4 weeks. Your doctor will follow up with you to ensure the fracture alignment doesn’t change and get worse during your healing process.
Fractures that are displaced may need to be treated with closed reduction and splinting. This involves manually moving the bones back into proper alignment and holding them in place with a splint. You will usually receive a local anesthetic prior to the reduction to decrease your pain. A splint will be used to ensure there is no motion at the fracture site. This splint will incorporate the wrist and the involved finger and neighboring finger out to the tips. These fractures are followed very closely and may need to be monitored weekly in the beginning to make sure things are staying well aligned. Your doctor will determine when you have sufficient healing and can discontinue wearing the splint. Healing depends on several factors including age, fracture type and severity, but most patients will be immobilized for about 4 weeks. Physical therapy will usually be a part of your recovery. Your hand may feel stiff and weak after the splint is removed and therapy will help you regain motion and strength.
Other displaced fractures that are unstable or in multiple pieces may need surgical intervention. Surgery may be done by putting a long screw into the canal of the metacarpal to realign the fracture or by using a plate and screw on the outside of the bone. The goal in both cases is to realign the bone and hold it in place with internal hardware. You will be placed in a splint after surgery. Often, you will remove the splint early on to begin range of motion exercises to avoid stiffness. Your fracture will not be healed at this point, but motion is safe because the hardware is keeping everything aligned. You will still be unable to do any strengthening or contact sports until the fracture is healed.

Interphalangeal Joint Fusion
Interphalangeal Joint Fusion in Wayne, Paramus, and Parsippany NJ
This is for severe painful arthritis with little to no preserved motion in the joint.\
Interphalangeal fusion is usually reserved for patients with severe painful arthritis with little to no preserved motion in the joint. The goal of a fusion is to eliminate pain caused by arthritis by fusing the two bones together, which will also subsequently eliminate any motion through the joint. This may be done in a variety of methods, but usually involves implanting hardware. The fusion may take six to eight weeks to fully heal, and your activities will be restricted until full healing has occurred.
Extensor Tendon Repair
Extensor Tendon Repair in Wayne, Paramus, and Parsippany NJ
The extensor tendon will likely need to be repaired to regain function and mobility.
After an extensor tendon rupture or laceration, the tendon will likely need to be repaired to regain function. The procedure should be done as close to the incident as possible to have the greatest chance of a solid repair, otherwise a tendon transfer or reconstruction may be needed. If a laceration was involved, the wound may need to be washed out and explored to avoid infection and to assess whether any nerve or vessel injuries occurred concurrently. After the tendon repair is complete, the hand will be immobilized. Further instruction will be given with regards to post-operative follow up in our office for removal of your dressing and protocol involving further immobilization, recovery and therapy. Closely following the instructions of your surgeon and therapist is critical because the tendon needs to be rehabilitated properly in order for you to regain motion and not compromise the repair. Each individual patient will have a rehab that is tailored specifically to their needs.
Basal Joint (Thumb) Arthritis
Basil Joint Arthritis Treatment in Wayne, Paramus, and Parsippany NJ
Basal joint arthritis is a degenerative process that takes place at the base of the thumb.
Basal joint arthritis is a degenerative process that takes place at the base of the thumb. It usually begins with intermittent pain in the thumb with repetitive or forceful motions. Patients may initially complain of pain with trying to open a tight jar or carrying a heavy load. As the arthritis progresses they may notice pain with opening doors, turning car keys, and may also feel a grinding sensation with thumb motion. Generally, the disease process starts gradually beginning with intermittent symptoms that may become more frequent over time. Basal joint arthritis can affect one or both hands, but many times symptoms will be noticed earlier on in the dominant hand. This type of arthritis can be addressed in many ways depending on the severity and dysfunction the patient is experiencing. We will discuss the treatment options in further detail, but first we want you to gain a simple understanding of the disease process.
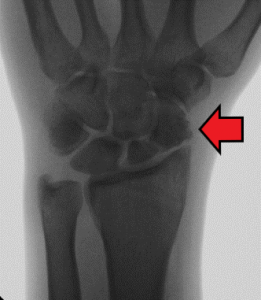
Cartilage is a smooth rubber-like tissue that cushions joint surfaces. Arthritis occurs when cartilage in a joint wears down. Eventually, the two bone surfaces are rubbing against each other when the joint moves. In basal joint arthritis, the base of the first metacarpal bone and the trapezium, a small carpal (wrist) bone beneath the thumb, begin to rub against each other. This rubbing is the source of the pain which may be felt as an aching, stabbing, or intermittent. Over time the space that was once between those bone disappears and they are resting against one another. Your thumb may feel weak and have decreased range of motion. This condition usually develops over time, but in some cases it may first be noticed after trauma or injury.Basal Joint Arthritis
Basal joint arthritis can be diagnosed through careful examination of the hands and thumbs. X-rays are helpful in obtaining a definitive diagnosis and gives your doctor a better idea of how far the arthritis has progressed. X-rays will clearly show that the space between the two bones has deteriorated and may reveal bone spurs as a result. Our offices are equipped with fluoroscopy machines that allow us to take low dose radiation images of the hand during your appointment.
Treatment of basal joint arthritis depends on the patient, the severity of symptoms, and the stage of the disease process. Usually, initial treatment is conservative and consists of bracing and cortisone injections. Cortisone injections are given into the joint and help to decrease inflammation and pain in the area. Many times patients will have long term relief following an injection, but in more advanced cases the relief may not last as long or at all. Our doctors will image your hand through fluoroscopy while doing the injection to ensure the cortisone is injected into the exact location of your arthritis. If symptoms persist or worsen over time you may be a candidate for surgery.
Surgery usually involves removing a small carpal bone called the trapezium that sits at the base of your thumb and is the source of pain in basal joint arthritis. Removal of this bone does not alter the mobility or function of the thumb but does alleviate your pain. Once that bone is removed, the thumb metacarpal will be suspended in a variety of ways that may involve a tendon transfer, pinning or a tight rope suspension. All of these are appropriate options, although some may allow for earlier motion than others. Your doctor will discuss the surgery they think is right for you.
Physical therapy will be a large part of your rehabilitation process regardless of the specific type of surgery done. Hand therapists in particular are specifically trained in this type of rehabilitation. They will design a therapy program that is tailored to your needs and goals. They may also make a custom splint that can be worn during the beginning stages of recovery if advised by your doctor. Certified hand therapists have a wide array of skills, tools, and modalities that are specific to regaining fine motor skills, hand strength, and dexterity.
Thumb arthritis can be extremely painful and cause serious dysfunction for patients. Our goal at Modern Orthopaedics is for you to return to the things you love! This may take time and patience, but we want you to experience a full recovery. We understand that every patient is unique and we will develop your treatment plans accordingly. We want to understand your goals and help you reach them. Please contact our office with any thumb or hand issues and receive superior care from our doctors and staff.
Basal Joint (Thumb) Arthroplasty
Basal Joint Arthroplasty in Wayne, Paramus, and Parsippany NJ
A procedure designed to alleviate thumb pain while preserving mobility and function of the thumb.
Surgery usually involves removing a small carpal bone called the trapezium that sits at the base of your thumb and is the source of pain in basal joint arthritis. Removal of this bone does not alter the mobility or function of the thumb but does alleviate your pain. Once that bone is removed, the thumb metacarpal will be suspended in a variety of ways that may involve a tendon transfer, pinning or a tight rope suspension. All of these are appropriate options, although some may allow for earlier motion than others. Physical therapy will be a large part of your rehabilitation process regardless of the specific type of surgery done.
Mallet Finger
Mallet Finger Treatment in Wayne, Paramus, and Parsippany NJ
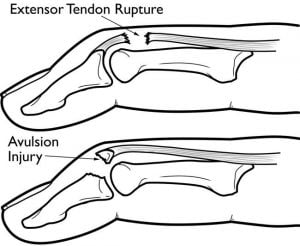
Mallet finger injuries occur when the extensor tendon and often a fragment of bone detaches from the distal phalanx.
Each of our fingers consist of three separate bones called phalanges. These bones articulate allowing each finger to bend in three places. Tendons are long, thin, flexible bands of fibrous connective tissue that attach muscle to the bone, allowing our fingers to bend and straighten. When a tendon is cut or ruptured the muscle will no longer be able to control your finger because the connection is lost. Mallet finger injuries occur when the extensor tendon ruptures from the distal phalanx. Often times an associated avulsion fracture can occur, meaning that a small fragment of bone detaches from the distal phalanx with the tendon.
Mallet finger is a common injury that can occur on the sports field, at work, or in the kitchen. Usually the patient will report that something hit the tip of their finger while it was in a bent position and then they were unable to straighten it. The finger may be sore, but sometimes people feel little pain and only notice that they are unable to straighten the tip of the finger. Our doctors can usually tell right away when this injury has occurred through examination of the finger. X-rays are often taken to determine whether there is bony involvement of the distal phalanx.
Mallet Finger
The goal of treatment in mallet finger is to get the tendon to heal back to the distal phalanx. If there is an associated avulsion fracture the treatment is essentially the same, but healing can occur sooner in these cases because the piece of bone attached to the tendon may aid in the healing process. Although mallet finger seems like a small and sometimes insignificant injury the healing process can feel long. The good news is that the vast majority of mallet fingers will heal without surgery.
Initial treatment is a strict splinting regimen for 6-8 weeks. This involves a splint that keeps the most distal finger joint in complete extension. The splint must be kept on and not removed throughout the healing process so that the distal interphalangeal (DIP) joint does not bend. If the tip of the finger bends, it can disrupt any healing that has occurred and you often have to start the 8 week process again. If you need help changing your splint or need a new splint during this time you can call our office for a splint change. You should keep the splint covered while showering or getting your hands wet to avoid the splint slipping off or irritation of the skin on the top of the finger.
Once the tendon heals back to the bone, the patient will begin to wean the splint and begin gentle range of motion exercises. In most cases, the patient may have a slight extensor lag (meaning the finger may be unable to fully straighten at the tip), but the finger is fully functional. Generally, physical therapy is not a necessary part of your recovery. Most patients can return to their activities soon after they wean the splint.
In rare instances, some patients may be unable to tolerate 8 weeks of strict splinting for mallet finger treatment. If this is the case, there is a surgery that can be done. This involves having a pin inserted across the distal interphalangeal joint to place the tendon in a place where it will heal. The pin will stay in place for 8 weeks. Most patients will still feel more comfortable wearing a splint during this 8-week period, but it may be removed without the fear of having stress put on the tendon as it heals. After 8 weeks the pin will be removed and the patient will regain motion in their DIP joint. This is done as a same day procedure at the hospital or in a surgery center. Physical therapy is usually not necessary, but may be used if there are issues regaining motion.
Mallet fingers can be very bothersome and pesky injuries. Our goal at Modern Orthopaedics is for you to return to the things you love! This may take time and patience, but we want you to experience a full recovery. We understand that every patient is unique and we will develop your treatment plans accordingly. We want to understand your goals and help you reach them. Please contact our office with any finger issues and receive superior care from our doctors and staff.
Mucous Cyst Excision
Mucous Cyst Excision in Wayne, Paramus, and Parsippany NJ
Excision of small cysts that grow over finger joints.
The surgery requires a small incision directly over the cyst. Dissection is taken down to the level of the joint, and the stalk of the cyst is excised. Additionally, any osteophytes are identified if present and then removed. The finger is usually placed in a soft dressing for the first few days after surgery. After this time, the dressing may be removed and the patient is encouraged to begin gentle range of motion. The stitches are removed after two weeks and the patient is cleared to return to all activities.
Formal therapy is generally not necessary; instead simple range of motion exercises can be performed at home. To keep your fingers moving, alternate between straightening and flexing each finger making sure to attempt to complete a full fist. This a simple yet important part of your recovery. It is also important to gently massage your surgical scar (after the first week) which will help soften and desensitize the healing tissue.
Flexor Tendon Repair
Flexor Tendon Repair in Wayne, Paramus, and Parsippany NJ
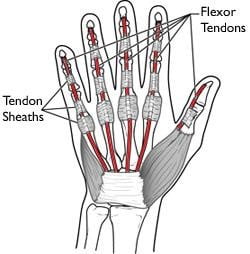
Surgical repair of a ruptured flexor tendon is commonly required to allow for regained flexion of the finger.
Complete flexor tendon ruptures or lacerations will require surgical repair to regain function of the affected finger. It is important that the repair is done in a timely manner and as close to the incident as possible to prevent the need for a more complex surgery. This surgery can be done as a same-day procedure in an ambulatory surgical center. After the tendon is repaired, the hand is splinted in a bent position to immobilize the fingers and keep tension off of the newly repaired tendon. Closely following the instructions of your surgeon and therapist is crucial during this post-operative phase, because the tendon must be rehabilitated properly in order to regain motion and not compromise the repair. Once adequate time is spent resting and healing the repair, your surgeon will progress you to formal physical therapy which is done in a gradual manner. Each individual patient will have a rehab protocol that is tailored specifically to their ability and needs.
DIP Pinning for Mallet Finger
DIP Pinning for Mallet Finger in Wayne, Paramus, and Parsippany NJ
Interphalangeal Arthritis
Interphalangeal Arthritis Treatment in Wayne, Paramus, and Parsippany NJ
Interphalangeal arthritis occurs in the fingers as a result of degenerative changes post traumatically, chronic wear or underlying inflammatory conditions.
Interphalangeal arthritis occurs in the fingers as a result of degenerative changes post traumatically, chronic wear or underlying inflammatory conditions. Over time, the cartilage wears down and the joint space narrows causing pain and swelling in the joint. Motion may be restricted and the patient may notice bony nodules surrounding the joint. Diagnosis may be made by x-ray that will show loss of joint space and may show osteophytes and joint degradation. If there is suspicion of an underlying systemic condition, it may be necessary to order blood tests. Treatment will begin conservatively with rest, anti-inflammatories and possibly an intraarticular cortisone injection. If a patient’s pain persists despite conservative management, they may be a candidate for surgery.


Extensor Tendon Rupture/Laceration
Extensor Tendon Rupture/Laceration Treatment in Wayne, Paramus, and Parsippany NJ
If an extensor tendon has ruptured or has been lacerated, you will be unable to actively straighten your finger.
Extensor tendons run along the back of your hand and allow you to straighten your fingers. These tendons may rupture due to trauma, bone spurs or from degeneration of the tendon over time. Extensor tendons are close to the skin surface and may also be cut as result of a hand laceration. You will be unable to actively straighten your finger if the tendon has ruptured or is lacerated. In this case, our surgeons may order an MRI to visualize the tendons and determine which tendons have been disrupted and the extent of the injury. In order to regain function of your fingers, you may need surgery, which can consist of either a tendon repair, reconstruction or transfer. Click here for more information on extensor tendon repair.

UCL and RCL Repair
UCL and RCL Repair in Wayne, Paramus, and Parsippany NJ
Flexor Tendon Rupture/Laceration
Flexor Tendon Rupture/Laceration Treatment in Wayne, Paramus, and Parsippany NJ
Injury to a flexor tendon of the hand results in the inability to bend the affected finger.
Flexor tendons of the hand are responsible for flexion (bending) of the fingers and are located on the palm side of the hand. Injury to one of these tendons creates an inability to bend the affected finger. Typically, these injuries occur due to deep cuts (lacerations) or if the tendons are place under high tension and rupture. Symptoms associated with this injury include the inability to bend one or more joints of the finger, pain when the finger is bent, tenderness to the tendon when pressure is applied and if the tendon was lacerated, an open wound with possible numbness to the fingertip. This is easily diagnosed in the clinical setting with a thorough clinical exam. Tendons cannot heal when completely torn and often require surgery to repair the affected tendon (See “Flexor Tendon Repair” found in the Treatments section). Once repaired, a period of rest is required to allow the repaired tendon to heal. Your surgeon will than start you on a gradually progressive physical therapy regimen to slowly regain motion and function of the finger.
Finger Mass/Cyst
Finger Mass/Cyst Treatment in Wayne, Paramus, and Parsippany NJ
Cysts or soft tissue masses can develop in the fingers and usually have no specific etiology. Most soft tissue masses are painless, but there are some that can cause pain. Glomus tumors, for example, are benign but painful and very sensitive to temperature change. Some masses may grow rapidly while others may be indolent and slow growing. Our hand specialists will examine and evaluate your issue and order the necessary testing to make a diagnosis. Some ganglion cysts can be aspirated in the office, but this does not guarantee that they will not recur. Ganglion cysts have a deeper stalk that will often cause the sac to reflate even after they have been drained. The most definitive treatment of any soft tissue mass or cyst is with a complete surgical excision and also gives you the best chance to avoid recurrence of the mass. Once the mass or cyst is excised, the specimen is sent to pathology to identify the exact origin for a definitive diagnosis.
Finger Mass/Cyst Excision
Finger Mass/Cyst Excision in Wayne, Paramus, and Parsippany NJ
Surgically excise a mass or cyst that has become bothersome or cannot be treated conservatively.
When a mass or cyst has become bothersome or cannot be treated conservatively, it may need to be excised surgically. Depending on the size and depth of the mass, this may be done under local anesthesia. The procedure involves making an incision directly over the mass and dissecting through the surrounding tissues to remove it. Sometimes an MRI may be required for preoperative planning to assess the exact location and depth of the mass. The specimen will be sent to pathology for a definitive diagnosis. Generally, the dressing may be removed two to three days after surgery. The sutures will be removed in the office about two weeks after surgery, and your surgeon will review your pathology results at that time.
Metacarpal (Hand) CRPP or PRIF
Metacarpal CRPP or PRIF Treatment in Wayne, Paramus, and Parsippany NJ
Metacarpal fractures may need stabilization with wires placed through the fracture site in the operating room or with internal hardware as plates and screws.
Metacarpal CRPP (Closed Reduction and Percutaneous Pinning)
Metacarpal fractures may need stabilization with wires placed through the fracture site in the operating room. Percutaneous pinning generally does not require an incision of any kind, and the pins are removed once the bone is healed. The bone will need to be immobilized while the pins are in place and the area needs to be kept clean and dry to avoid infection. Once the bone is healed and the pins are removed, the patient will need to regain their motion either on their own or with the help of formal physical therapy.
Metacarpal (ORIF) Open Reduction Internal Fixation
Some metacarpal fractures are best treated with open reduction and internal fixation (ORIF). This requires an incision and application of internal hardware in the form of plate and screws or an intramedullary screw to stabilize the bones. This hardware generally stays in place and is not removed. It still takes four to six weeks for the fracture to heal, but often range of motion can be started sooner because the fracture is stabilized from the inside. X-rays will be taken during your follow up appointments to ensure maintained alignment and healing of the fracture.
Mucous Cyst
Mucous Cyst Treatment in Wayne, Paramus, and Parsippany NJ
Mucous cysts most commonly occur over the most distal joint of the finger.
Mucous cysts most commonly occur over the most distal joint of the finger. Distal interphalangeal (DIP) joint arthritis may cause bone spurs to develop in this area and mucous cysts may form. They usually appear as a bump on either side of the finger joint. They are often tender and fluid filled. The fluid inside the cyst is originating from the DIP joint. You should not attempt to drain the fluid on your own, because it is in direct communication with the joint and a serious joint infection could develop.
X-rays may be taken to determine the extent of the arthritis and identify any osteophytes (bone spurs) that have developed. If the mucous cyst is significantly bothersome or threatening to drain, surgical intervention is indicated.

UCL and RCL Rupture
UCL and RCL Rupture Treatment in Wayne, Paramus, and Parsippany NJ
Injury to the ligaments that help stabilize the fingers.
Ulnar collateral and radial collateral ligament injuries in the fingers generally occur at the metacarpophalangeal (MCP) joints. These ligaments help to stabilize the fingers and most importantly the thumb at this joint. This injury can occur in any of the fingers when an overwhelming stress is placed in either the radial or ulnar direction at the joint, but it most commonly occurs in the thumb. Gamekeeper’s thumb occurs when the ulnar collateral ligament of the thumb is ruptured, allowing the thumb to deviate beyond its endpoint when stressed in a radial direction. This may or may not involve an avulsion of the bone, meaning a small fleck of bone pulled off with the ligament. Sometimes, a “Stener” lesion will occur in which the ligament becomes displaced above the adductor aponeurosis and will not heal without surgery. Treatment depends on the severity and location of the tear. Often widening may be seen at the location of the tear with stress view x-rays. An MRI is the most definitive way to determine the extent and location of the tear. If the ligament is in good position for healing, the patient may start with conservative management which is strict immobilization for 4-6 weeks.

Darrach and Sauve-Kapandji Procedures
Darrach and Sauve-Kapandji Procedures in Wayne, Paramus, and Parsippany NJ
Darrach Procedure
A Darrach procedure is reserved for patients with chronic DRUJ (distal radioulna joint) instability or DRUJ arthritis. This surgical procedure involves resection of the ulnar head which eliminates the rubbing of the distal portion of the ulna on the sigmoid notch of the radius.
Sauve-Kapandji Procedure
Sauve -Kapandji procedure involves fusion of the ulnar head to the radius and resection of a portion of the distal ulnar shaft. This allows the structures of the TFCC to remain intact while eliminating pain at the DRUJ. Resecting a portion of the distal ulnar shaft preserves the ability of the arm to supinate and pronate (turning your palm up and down).
Trigger Finger
Trigger Finger Treatment in Wayne, Paramus, and Parsippany NJ
Trigger finger is a bothersome clicking or locking of the finger.
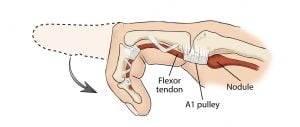
Trigger finger is a problem that can develop over time. There is usually no one specific cause of this disorder; however, it does occur more frequently in diabetics. This pathology may cause a bothersome clicking or locking of your finger that can be painful at times, and patients may not be able to straighten the finger without using assistance from the other hand. You may even feel a small painful nodule at the base of your finger. The snapping or clicking that’s felt is a result of inflammation surrounding the flexor tendon in your finger, whereas a normal tendon glides smoothly through several pulleys. When inflammation develops, the tendon may get stuck on the wrong side of the pulley and prevent you from straightening the finger.
Treatment for this condition usually begins with a corticosteroid injection. This injection has anti-inflammatory properties which should allow the inflammation surrounding the tendon to subside. If a corticosteroid is not successful after two attempts and the issue is persisting, then you may be a candidate for surgery.
Trigger Finger Release
Trigger Finger Release in Wayne, Paramus, and Parsippany NJ
The pulley is released to allow the finger tendon to glide smoothly.
If a corticosteroid injection does not successfully treat your trigger finger after two attempts, then you may be a candidate for either percutaneous trigger finger release or open trigger finger release.
Percutaneous trigger finger releases can be done in the office. The finger of interest must be reproducibly triggering so that we are able to determine whether or not the pulley is successfully released. Local anesthesia is given, and a small poke hole is made in the skin. A needle is used to cut and release the pulley that the tendon is getting caught on. The finger is then tested to ensure that it is no longer getting caught. A compressive dressing is placed for the patient to wear over the next few hours. The area may be sore for a few weeks while everything heals. Hand and finger range of motion is encouraged immediately after the procedure. This is only an option for certain patients depending on the finger involved and the severity of the triggering.
The open trigger finger release may also be done under straight local anesthesia, but this procedure is done at a hospital or ambulatory surgery center. It involves making a small incision at the base of your finger over the involved pulley. The pulley is cut so that your tendon will glide smoothly without getting caught. A soft dressing is placed after surgery that may be removed after two to three days. Stitches will be removed in the office two weeks after surgery. Hand and finger range of motion is encouraged immediately after surgery, and full recovery usually takes a few weeks.
Ganglion Cyst Excision
Ganglion Cyst Excision in Wayne, Paramus, and Parsippany NJ
Ganglion cyst excisions are usually done with a small open procedure directly over the cyst. On some occasions, they are removed arthroscopically depending on the cyst’s location and size. Once the cyst is visualized, instruments are used to excise the cyst sac all the way down to the stalk. Removing the cyst stalk helps to ensure that they cyst will not recur. Generally, you will wear a small splint for the first week after surgery. Once the splint is removed, you will begin to regain your motion and strength frequently with a home exercise program. Full recovery generally takes a few weeks, although you may return to most activities as tolerated after your first follow up visit.

Ulnar Shortening Osteotomy or Wafer Procedure
Ulnar Shortening Osteotomy or Wafer Procedure in Wayne, Paramus, and Parsippany NJ
If a patient has positive ulnar variance and persistent pain despite conservative management, they may be a candidate for an ulnar shortening procedure. This can be done through a wrist arthroscopy often performed at the same time as a TFCC debridement or repair. The procedure involves using an instrument to shave down the most distal portion of the ulnar head so that it no longer impacts the carpal bones. An ulnar shortening osteotomy involves cutting out a piece of the ulnar shaft to shorten the whole bones and fixing it with a plate and screws. In this case, the bone needs to heal at the site it was cut before the patient can return to activities.
Wrist, PRC, and Four Corner Fusion
Wrist, PRC, and Four Corner Fusion in Wayne, Paramus, and Parsippany NJ
Total or Partial Wrist Fusion
A partial wrist fusion involves fusing the radiocarpal joints that have been most affected by arthritis, while a total wrist fusion involves fusing the whole radiocarpal joint. This may be done with screws, plates or staples. In this case, the patient will be sacrificing wrist motion for pain relief. Recovery will involve immobilization for about six weeks while the fusion heals.
Four Corner Fusion
A four corner fusion is one technique in which midcarpal arthritis can be addressed surgically. This procedure involves removing the scaphoid bone and fusing together four of the remaining carpal bones. This is usually reserved for patients with a well preserved radiolunate joint and isolated midcarpal arthritis. The capitate, lunate, hamate and triquetrum are fused together with screws or large metal staples. This eliminates motion between these bones but preserves some motion at the wrist. These bones will fuse together into one bone with no joint space over time. The goal of this surgery is to eliminate pain caused by midcarpal arthritis and allow the patient to return to having a functional pain free hand and wrist.
Proximal Row Carpectomy
A proximal row carpectomy involves removing the scaphoid, lunate and triquetrum bones. This may be used in patients with Kienbock’s disease (avascular necrosis of the lunate), scaphoid nonuion, SLAC (scaphoid lunate advanced collapse) or SNAC (scaphoid nonunion advanced collapse) wrist. It is usually not a good option for patients with advanced arthritic changes. The goal of the surgery is to remove the bones causing pain while allowing the patient to retain some motion. The recovery time is generally quicker following this procedure, because you do not need to wait for any bones to fuse or heal before returning to activities.
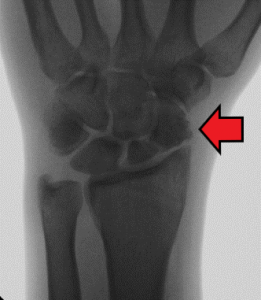
Scaphoid Fracture Open Reduction Internal Fixation (ORIF)
Scaphoid Fracture Open Reduction Internal Fixation (ORIF) in Wayne, Paramus, and Parsippany NJ
Sometimes surgery is indicated to treat a scaphoid fracture whether it is an acute problem or a long-term problem. A scaphoid nonunion occurs when a scaphoid fracture is chronic and has not healed properly. This may cause pain and can lead to an issue called scaphoid nonunion advanced collapse or SNAC wrist. In either an acute or chronic case, the fracture is reduced and internal hardware is inserted to keep the fracture in proper anatomic alignment. Bone graft may or may not be used to augment healing. Strict immobilization is very important after surgery to ensure proper healing of the bone. Once the bone is healed, the patient will begin exercises to regain motion and strength.
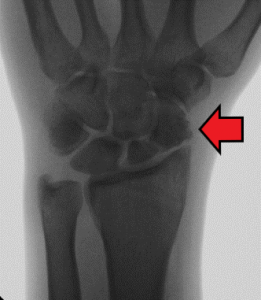
De Quervain’s Release
De Quervain’s Release in Wayne, Paramus, and Parsippany NJ
If a patient has attempted conservative management and failed to achieve pain relief, they may be a candidate for a first dorsal compartment release. This procedure can be done under local anesthesia in a hospital or ambulatory surgery center. It involves an incision over the thumb side of the wrist. The first dorsal compartment will be identified and released to open the tunnel and free the tendons. After surgery, a splint may be applied for about one week to rest the wrist. After one week, the splint is removed and you will begin to regain your motion and strength with a series of hand and wrist exercises often able to be performed at home. Recovery generally only takes two to three weeks, and you can return to most activities as tolerated after your first follow up appointment.
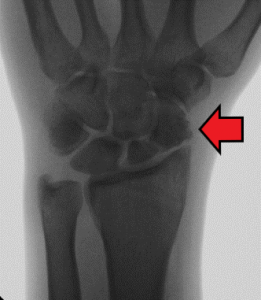
Both bone forearm Open Reduction Internal Fixation (ORIF)
Scaphoid Fracture Treatment in Wayne, Paramus, and Parsippany NJ
Both bone forearm fractures may need to be treated with open reduction and internal fixation. This may be done with intramedullary rods, more commonly in children, or plates and screws. The goal of surgery is to reduce the fractures to their proper anatomic alignment and keep them aligned with internal hardware. It will still take four to six weeks for the bones to heal, but the hardware ensures that they maintain anatomic alignment while the healing process takes place and therefore avoid improper healing which can cause future pain and dysfunction.


Distal Radius (Wrist) Fractures
Orthopedic Distal Radius Fracture Surgery in Wayne, Paramus, and Parsippany NJ
A fracture of the distal radius (wrist fracture) usually occurs from a fall onto an outstretched hand.
The wrist joint consists of eight small carpal bones in the hand that connect to the radius and ulna bones in the forearm. This joint allows for extensive movement and manipulation of the hand. The wrist is often injured if you fall onto an outstretched hand or put your hand behind you when falling backward. The radius, the larger of the two bones in the forearm, is most commonly fractured near the area where it meets the wrist. Many different types of radius fractures can occur.
A patient with a distal radius fracture will generally present with a history of trauma, pain in the wrist, swelling, and inability to move the wrist or bear weight on the hand. If a fracture is more severe they may have a visible deformity or the wrist may appear crooked. If you have any or all of these symptoms, you should be seen by an orthopedic doctor for evaluation.
Our doctors will examine your wrist and order an x-ray to determine the location and severity of your fracture. Sometimes a CT scan will be necessary to evaluate a complex fracture. Some nondisplaced fractures can be treated with a splint or a cast. Nondisplaced means that there is a visible fracture, but the alignment of the radius is unchanged. The fracture will be followed by serial x-rays to ensure there is no displacement or movement of the fracture site.These fractures will generally heal with 4 weeks of immobilization. At that point, if there is adequate healing and no tenderness over the fracture site, you can begin gentle wrist range of motion and return to activities gradually. Physical therapy is sometimes required as a part of you rehabilitation, although our doctors will determine if they think it is necessary.
A displaced distal radius fracture may need to be treated with closed reduction and splinting. This involves administering numbing medication into the wrist and manually moving the bones back into proper alignment. The fracture is then held in place with a splint. A sugar tong splint will often be used to ensure there is no motion at the fracture site. This splint starts at the hand and goes up and over the elbow.
If you have any or all of these symptoms, you should be seen by an orthopedic doctor for evaluation.
Our doctors will examine your wrist and order an x-ray to determine the location and severity of your fracture. Sometimes a CT scan will be necessary to evaluate a complex fracture.
These fractures are followed very closely and may need to be monitored weekly, in the beginning, to make sure things are staying well aligned. Your doctor will determine when you have sufficient healing and can discontinue wearing the cast. Healing depends on several factors including age, fracture type, and severity, but most patients will be immobilized for 4-6 weeks.
Surgery is often needed for distal radius fractures that involve the joint, are in multiple pieces, or are unstable. Your doctor will order necessary imaging prior to surgery to ensure they understand the fracture pattern and are prepared to fix your fracture. Your fracture will likely be fixed with a plate and screws that sit on the bone and hold the fracture in place.
This allows your bone to heal in the proper position so that you are less likely to have issues with motion and strength in the future. The hardware will generally stay in the wrist for the patient’s lifetime. On occasion, a patient may be bothered by the hardware in which case it can be removed with a subsequent surgery once the bone is completely healed. After surgery, you will be placed in a splint and follow up in our office in 1-2 weeks. At that point, new x-rays will be taken and the splint will likely be removed. Your doctor may place you in a removable brace and instruct you to start gentle range of motion, depending on your progress. Physical therapy is generally a part of your recovery. You will start with simple range of motion exercises and progress to strengthening when prescribed by your doctor.
Distal radius fractures can cause serious setbacks for patients of all ages. Our goal at Modern Orthopaedics is for you to return to the things you love! This may take time and patience, but we want you to experience a full recovery. We understand that every patient is unique and we will develop your treatment plans accordingly. We want to understand your goals and help you reach them. Please contact our office with any wrist issues and receive superior care from our doctors and staff.
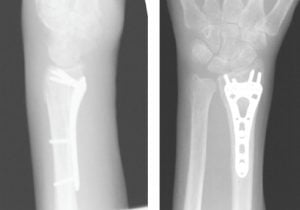
Both Bone Forearm Fracture
Forearm Fracture Treatment in Wayne, Paramus, and Parsippany NJ
Both bone forearm fractures occur when both the ulnar and radius break, usually the result of direct trauma or a high-energy fall. A diagnosis is made by x-ray, and treatment is determined by the severity of the fracture, the patient’s age and their medical condition. If the fractures are not displaced and can be adequately immobilized, the fracture can be treated in a splint or cast. Other fractures that are displaced, unstable or open need to be treated with surgery. Please refer to our “Treatments” section for more information.

Carpal Tunnel Syndrome
Carpal Tunnel Syndrome Treatment in Wayne, Paramus, and Parsippany NJ
Carpal tunnel syndrome usually begins with symptoms of numbness, tingling, or burning in one or both hands. Some patients wake up at nighttime with pins and needles in their fingers, others may feel their hands fall asleep when they are driving, and some may feel sudden jolts of “electricity” in the hand when doing heavy labor. Carpal tunnel syndrome can present with a wide array of symptoms, but it is a very common issue. Generally, the disease process starts gradually beginning with intermittent symptoms that may become more frequent over time.
Once the disease process has progressed, patients may notice difficulty with fine motor skills such as buttoning a shirt or picking up coins. Addressing carpal tunnel syndrome at or near its onset is most beneficial and will help ensure no permanent loss of muscle or sensation. There are several different treatment options that we will discuss in further detail, but first, we want you to gain a simple understanding of the disease process.
What Is Carpal Tunnel Syndrome?
Carpal tunnel syndrome is a compression of the median nerve at the wrist level. The median nerve is a long nerve that runs down your arm and into your hand. It is in charge of sensation in the hand as well as different motor functions. The carpal bones are bones in the hand that create a crescent that many tendons and your median nerve run through. The transverse carpal ligament creates a roof for the crescent and encloses the tendons and median nerve.
During carpal tunnel syndrome the pressure within this fixed space increases and begins to compress the median nerve. This pressure increase can be due to overuse, inflammation of the tendons, trauma, or other factors. The median nerve is very sensitive to these pressure changes and when compressed may cause weakness, numbness, and tingling into your hand. If compressed for long periods you may develop muscle atrophy and damage that is difficult to reverse. It is important to have your carpal tunnel syndrome evaluated to determine its severity and your best course of treatment.
How Do I Know If I Have Carpal Tunnel Syndrome?
Carpal tunnel syndrome can be diagnosed through careful examination and special tests that our doctors will perform in our office. Depending on the severity of your symptoms, our doctors may order nerve studies from a neurologist to help delineate the extent of nerve compression and damage, although this is not always necessary.
Treatment for mild carpal tunnel syndrome may start conservatively. Wearing supportive wrist braces at night is often an initial step. This will help keep your wrists in a neutral position, avoiding wrist flexion and further compression of the nerve. A corticosteroid injection may also be offered to help alleviate inflammation and symptoms. Operative treatment may be offered if you have a moderate or severe case of nerve compression or if conservative treatments have been exhausted and your symptoms persist.
De Quervain’s Tenosynovitis
Wrist Tendonitis Surgery in Wayne, Paramus, and Parsippany NJ
De Quervain’s tenosynovitis produces pain over the thumb side of the wrist.
There are many different tendons that run over and under the wrist. These tendons allow for our fingers and wrist to bend and straighten. Each tendon has a unique location and function. DeQuervain’s tenosynovitis affects the abductor pollicus longus and extensor pollicus brevis tendons which help control thumb motion. DeQuervain’s tenosynovitis is a common tendon issue in the wrist and can affect patients both young and old. Patients may complain of pain when lifting their newborn, often referred to as “Mommy thumb”, others may notice the pain while doing repetitive lifting at their job or while doing house work, and some may notice the pain while texting or using their phone.
DeQuervain’s tenosynovitis / Wrist TendonitisPatients generally present with pain over the thumb side of the wrist. This area is called the first dorsal compartment of the wrist. This compartment contains the abductor pollicus longus and extensor pollicus brevis tendons. There may be visible swelling directly over this area and it may be tender to touch. Inflammation of the soft tissues surrounding the tendons in this compartment may cause narrowing and pain. Pain will commonly be elicited with any kind of lifting, pinching or grasping activity in ulnar deviation and with use of the thumb. Our doctors can usually make a diagnosis on physical examination alone. Once the diagnosis is established they will discuss the different treatment options.
Generally, initial treatment involves immobilization of the wrist and thumb with a soft brace. These thumb spica braces are available in our office or a custom brace may be made by a hand therapist. The brace allows the tendons to rest, helps alleviate pain and hopefully decreases inflammation in that area. It is also common that a cortisone injection will be offered at your initial apppintment. The cortisone is injected directly into the first dorsal compartment and surrounding the affected tendons. Cortisone is a steroid that works to decrease inflammation in that area. Patients will usually feel relief within a couple of days after the injection. If the pain does not respond to the cortisone injection or recurs, then surgical intervention may be indicated.
Surgical treatment for DeQuervain’s tenosynovitis is a straightforward and quick treatment although our doctors will continue to take the utmost care during this procedure. The procedure can be done under local anesthesia in a hospital or ambulatory surgery center. This means that a numbing injection will be given into the area of the wrist where the surgery is done, but otherwise you will be awake. You will not feel any pain and by avoiding general anesthesia you will not need to spend extra time in the recovery room time once the surgery is over. If you have any concerns about being awake during the procedure you can certainly discuss with you doctor other options.
During the surgery an incision is made over the thumb side of the wrist. The first dorsal compartment will be identified and released to open the tunnel and free the tendons. After surgery, a splint may be applied for about one week to rest the wrist. After one week, you will follow up in our office and the splint will be removed. At this point, you will begin to regain your motion and strength with a series of hand and wrist exercises. Generally these exercises can be done on your own at home, although formal physical therapy may also be recommended. Recovery generally takes two to three weeks, and you can return to most activities as tolerated within that time.
DeQuervain’s tenosynovitis can be extremely frustrating and cause serious setbacks and dysfunction for patients. Our goal at Modern Orthopaedics is for you to return to the things you love! This may take time and patience, but we want you to experience a full recovery. We understand that every patient is unique and we will develop your treatment plans accordingly. We want to understand your goals and help you reach them. Please contact our office with any wrist issues and receive superior care from our doctors and staff.
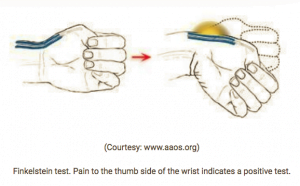
Dupuytren’s Contracture
Dupuytren’s Contracture Treatment in Wayne, Paramus, and Parsippany NJ
Dupuytren’s contractures develop as a result of the thickening of palmar fascia in your hand. Cords may begin as a thick area of tissue in the palm or finger, but over time they may pull the fingers down and prevent the fingers from fully straightening. This deformity is more common in people with Northern European heritage. There is no specific known cause of the development of the contractures. It is easily diagnosed upon physical examination by a hand specialist. Usually the cords develop slowly and sometimes they may remain as a small painless nodule that doesn’t affect finger extension. If this is the case, there is generally no treatment that is needed. Over time the cord may begin to tether the fingers down and affect hand function. Once the bands begin to cross the finger joints causing contractures that affect daily life the patient may be a candidate for treatment with Xiaflex injections. See our “Treatments” section for more on “Xiaflex injections.”
DRUJ Instability/Arthritis
DRUJ Instability/Arthritis Treatment in Wayne, Paramus, and Parsippany NJ
The distal radioulnar joint (DRUJ) is located between the ulnar head and the sigmoid notch of the radius. It is stabilized by various ligaments and the TFCC (triangular fibrocartilage complex). It can become unstable most commonly after distal radius fractures or TFCC tears (“See TFCC tear” for more information). Some symptoms associated with this condition are pain with forearm rotation, crepitus, snapping/clicking sensation and decreased grip strength. Radiographs can help diagnose your condition by showing widening at the DRUJ or ulnar head subluxation. Sometimes more advanced imaging is also used to evaluate the injury. This may be treated in a variety of ways depending on whether your injury is acute or chronic. Sometimes simple immobilization will be sufficient, while other times operative intervention may be necessary.
In other cases, arthritis may develop in the DRUJ over time. This can be diagnosed with careful examination and x-rays. On x-rays the DRUJ may be narrow and there may be degenerative changes within the joint. This may lead to pain, crepitus and weakness in the wrist. Treatment may involve immobilization, cortisone injections or ultimately surgical intervention. See our “Treatments” page for more information.

Ganglion Cysts
Ganglion Cyst Treatment in Wayne, Paramus, and Parsippany NJ
Scaphoid Fracture
Scaphoid Fracture Treatment in Wayne, Paramus, and Parsippany NJ
The scaphoid is one of the eight carpal bones in the hand located on the thumb side of the wrist. It is commonly fractured but at times difficult to detect on initial x-rays and is often overlooked. Careful examination is important, and appropriate treatment is crucial to ensure healing. If the bone is not displaced, it can be treated with strict immobilization for 4-6 weeks, or in some cases longer, to heal. If the bone does not heal or if the fracture is displaced, surgery may be indicated to avoid future dysfunction and pain.
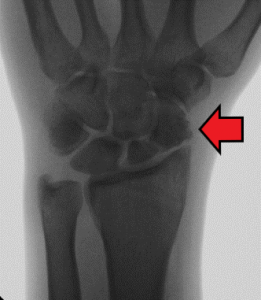
TFCC Tear Complex
TFCC Tear Complex Treatment in Wayne, Paramus, and Parsippany NJ
The wrist joint consists of eight small carpal bones in the hand that connect to the radius and ulna bones in the forearm. This joint allows for extensive movement and manipulation of the hand. The TFCC, triangular fibrocartilage complex, helps stabilize the distal radioulnar joint. It is made up of several ligaments and cartilage. There is a small articular disc in the center of the complex that cushions the wrist. Injury to the TFCC involves tears of the articular disc and surrounding ligaments. This injury can occur from an accident, falling onto an outstretched hand, repetitive wrist hyperextension and degenerative changes. Patients with positive ulnar variance, meaning the ulna is longer than the radius, are also more predisposed to TFCC injuries. This can be a result of a normal anatomic variant or from prior trauma. This relative difference causes the longer ulna to “abut” into the carpal bones, most commonly the lunate. This “impaction” can eventually cause TFCC tears along with other issues.
Pain from a TFCC tear is usually localized to the small finger side of the wrist, although in some cases the pain can be more diffuse. It is usually aggravated by any type of forearm rotation. Sometimes, patients may feel instability or catching inside the joint. Tears are diagnosed by a combination of history, clinical testing and MRI. Contrast is sometimes used during the MRI to help visualize the tear better, but this is not always necessary.
At your initial evaluation, you doctor will examine your wrist and do specific tests to assess the location of your pain and any instability you may have. X-rays will be done in the office to determine any potential abnormalities. If a TFCC tear is suspected your doctor will likely order an MRI to evaluate the extent and location of the tear. An MRI allows your doctor to see cross sectional images of the wrist and the surrounding tissues. Our doctors will ask that you bring a copy of your MRI to your next appointment so they can personally review the images. They will be able to look through the images with you and show you the source of your pain and the extensiveness of your injury.
There are different grades of TFCC tears, but treatment usually begins conservatively with immobilization and possibly a cortisone injection. Sometimes with rest and the help of cortisone to decrease inflammation in the area the pain may resolve. If the patient’s symptoms have not improved with conservative management or the patient is experiencing instability, they may be indicated for an arthroscopic TFCC debridement or repair.
A wrist arthroscopy involves using small cameras to see inside the wrist joint, assess the problems firsthand and treat them accordingly. Sometimes the TFCC needs to simply be debrided, which means cleaning up frayed pieces of damaged tissue. Other times the TFCC is torn and needs to be repaired with sutures. In the case where a repair is performed, you will be immobilized for a total of six weeks after surgery to allow for the repaired tear to heal. For the first few weeks you will be in a sugar tong splint that incorporates the wrist and the elbow. This prevents you from moving the wrist and rotating the forearm, which could affect your repair. At 2-3 weeks post op you will be transitioned into a Muenster cast which will allow for more movement of the elbow, but will still immobilize the wrist. After 6 weeks, you will be transitioned to a removable brace and begin formal physical therapy. Physical therapy will play a huge role in your recovery. You will being with range of motion exercises and progress to strengthening when your doctor thinks you are ready. Patients can generally return to most of their activities within 3-4 months of surgery. Although, it may take longer to return to sports that require heavy lifting or full weightbearing on the wrist.
TFCC tears can cause serious pain and dysfunction for patients of all ages. Our goal at Modern Orthopaedics is for you to return to the things you love! This may take time and patience, but we want you to experience a full recovery. We understand that every patient is unique and we will develop your treatment plans accordingly. We want to understand your goals and help you reach them. Please contact our office with any wrist issues and receive superior care from our doctors and staff.
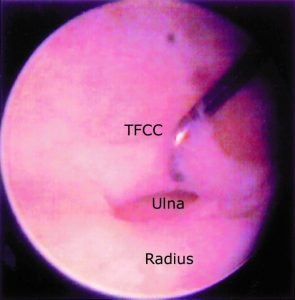
Finger Infections
Finger Infections Treatment in Wayne, Paramus, and Parsippany NJ
There are several types of finger infections, and it is important to understand the differences. Fingertip infections, also known as felons, are located at the fingertip pad. A paronychia is an infection that involves the soft tissue that surrounds the fingernail. Septic tenosynovitis of the finger is an infection of the fluid-filled sheath that surrounds the tendons. Finger infections can be very painful and persistent. Most finger infections are due to bacteria; however, fungal infections are also commonly seen. Initially these infections may be treated with oral antibiotics, antifungal medication if a fungal infection is suspected and warm soaks. If an abscess develops, it should be drained as a more definitive treatment. If the infection persists despite drainage and antibiotics, it may be necessary to surgically irrigate and debride the infected tissue. In the case of a paronychia, we remove the nail and cut the tissue just beneath the nail(eponychium) to allow complete resolution of the infection. Similarly, septic tenosynovitis often requires an incision, drainage and irrigation of the infected tendon sheath. Our hand specialists can address this issue in our office through clinical examination, imaging and drainage when needed. If the issue requires surgery, it may be done as a same-day procedure at a local hospital or surgery center.
Ulnocarpal Impaction
Ulnocarpal Impaction Treatment in Wayne, Paramus, and Parsippany NJ
Ulnocarpal impaction occurs when the distal ulna and carpal bones, primarily the lunate, bump into one another and cause pain. This may be caused by positive ulnar variance, radial shortening from a previous distal radius fracture or ligament tears. Pain is usually on the pinky side of the wrist and is worse with activities that cause ulnar deviation of the wrist. Radiographs may show positive ulnar variance, meaning the ulna bone is higher than the radius, and possibly sclerosis of the lunate bone or ulnar head from impaction. This also may predispose patients to TFCC tears. Conservative management consists of bracing and cortisone injections, although a surgical procedure may be the best option if pain and dysfunction persist.

Wrist Arthritis
Wrist Arthritis Treatment in Wayne, Paramus, and Parsippany NJ
Wrist arthritis commonly occurs post traumatically or from chronic and repetitive wear. Symptoms generally occur as pain and swelling in the wrist, along with decreased range of motion, ultimately effecting the patient’s overall function. The exact type and degree of wrist arthritis is best diagnosed with radiographs which can help pinpoint the joint surfaces and bones that are most involved. Management begins conservatively with bracing, NSAIDs and cortisone injections. If the pain persists despite conservative management, the patient may be a candidate for surgery. Surgical intervention consists of fusing specific joints in the wrist or hand. Removing certain carpal bones may be indicated as part of the procedure to eliminate the associated pain. A total wrist fusion, a partial wrist fusion, a four corner fusion or a proximal row carpectomy are some of the options available depending on the exact location and severity of the arthritis. Our orthopaedic hand specialists will determine which, if any, procedure would be best to treat your wrist for your lifestyle and needs.
SNAC Wrist
Scaphoid nonunion advanced collapse (“SNAC wrist”) occurs after sustaining a scaphoid fracture that goes undiagnosed or does not heal. Patients may present with a history of an old injury with complaints of wrist pain, stiffness and weakness. Diagnosis is often made with radiographs that show a scaphoid nonunion and the progression of the collapse. Treatment of this condition begins conservatively with bracing and cortisone injections, but definitive treatment requires surgery.
SLAC Wrist
Scaphoid lunate advanced collapse (“SLAC wrist”) usually occurs as the result of a chronic scapholunate ligament injury. Loss of stability between these carpal bones causes the scaphoid to go into a flexed position and the lunate to be extended. Over time, these abnormal forces and instability lead to arthritic changes between the radiocarpal and midcarpal joints. Patients may present with a history of an old injury and complaints of wrist pain, stiffness, and weakness. Diagnosis is often made with radiographs that will show scapholunate widening, radiocarpal and/or midcarpal arthritis, and a DISI (dorsal intercalated segment instability) deformity.

Arthroscopic TFCC Repair
Arthroscopic TFCC Repair in Wayne, Paramus, and Parsippany NJ
If your symptoms have not improved with conservative management then you may be a candidate for an arthroscopic TFCC (triangular fibrocartilage complex) debridement or repair. This involves using small cameras to see inside the wrist joint, assess the problem firsthand and treat it accordingly. Sometimes the TFCC needs to simply be debrided, which means cleaning up frayed pieces of damaged tissue. Other times the TFCC is torn and needs to be repaired with sutures. In the case where a repair is performed, you will be immobilized for a total of six weeks after surgery to allow for the repaired tear to heal. Thereafter, you will begin therapy to regain motion and strength.
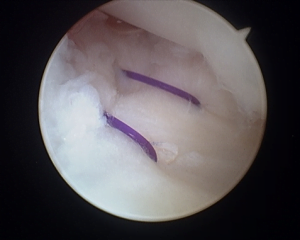
Hip
Conditions & Procedures
Femoroacetabular Impingement (FAI)
Femoroacetabular Impingement (FAI) Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
FAI is a congenital abnormality in which there is abnormal bone growth/formation of the bones that make up the hip joint.
Femoracetabular impingement (FAI) is caused by abnormal bone growth/formation of the bones that make up the hip joint — the femoral head (ball) and the acetabulum (socket). FAI occurs because the hip bones form abnormally during childhood. There are three types of FAI: pincer — bone growth over the rim of the acetabulum; cam — abnormally shaped femoral head; and combined impingement — both pincer and cam type impingement are present. Symptoms can take several years or decades to present, but when they do, it often indicates that there is damage to the cartilage or labrum due to the abnormality. Symptoms often present as pain in the groin, stiffness and limping. A thorough examination in the office coupled with imaging can confirm this diagnosis. Conservative treatment is often initiated as first-line therapy, implementing lifestyle modifications, physical therapy and anti-inflammatory medication. If conservative treatment fails or pain progresses to a severity that effects daily living, arthroscopic surgery may be indicated as the first-line surgical intervention utilized. During this procedure, the surgeon can remove frayed or damaged areas to the labrum and articular cartilage and shave down the bony abnormalities. In some cases, an open surgical approach may be necessary to accomplish this in order to establish adequate pain relief.

Hip Fracture
Hip Fracture Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Hip fractures are breaks in the upper quarter of the thigh bone (femur).
Hip fractures are breaks in the upper quarter of the thigh bone (femur) and are often seen with high-impact trauma directly to the hip in younger adults or from a fall to the hip in the geriatric population or those with medical conditions that can affect the integrity of the bone (i.e. osteoporosis, cancer). Symptoms often are acute and present as severe pain to the hip and groin area with any movement and an inability to walk. Often the effected limb will appear shortened and rotated as a result. Imaging can confirm this diagnosis, and in some cases advanced imaging may be utilized to evaluate the fracture. There are three types of hip fractures, and it is important for your surgeon to determine exactly which type of fracture is present, as the type of treatment is determined by the type of fracture, location and fracture pattern, and patient’s medical condition. If the patient is medically stable for surgery, surgical intervention is often recommended for an optimal prognosis. Rehabilitation with physical therapy is an important aspect to the recovery process.

Hip Arthritis
Hip Arthritis Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Hip arthritis is common and often occurs as we advance in age from chronic “wear-and-tear” of the joint where the cartilage damages and wears away over time.
Hip arthritis is common and often occurs as we advance in age from chronic “wear-and-tear” of the joint where the cartilage damages and wears away over time, decreasing the protective joint space between the femoral head (ball) and acetabulum (socket). This type of arthritis is known as osteoarthritis. Often, degenerative changes can be seen on x-ray as joint space narrowing and osteophytes (bone spurs). Arthritis in the hip can also be caused by inflammatory conditions, after trauma to the joint, or due to a congenital abnormality, but these types of arthritis are less common. Pain from arthritis in the hip may be felt directly at the hip, but often pain can be referred to the groin, down the thigh, at the level of the knee and can also be referred posteriorly to the buttocks or lower back. As arthritis progresses, you may experience loss of motion at the hip, crepitus, limping, tenderness and difficulty leaning on the effected side. Nonsurgical treatment is standard as the initial treatment for hip arthritis, often done by implementing lifestyle modifications, physical therapy and cortisone injections. If conservative treatment fails or the arthritis in the hip is severe causing significant pain and limitations of everyday life, you may be a candidate for a total hip arthroplasty (frequently referred to as a total hip replacement).
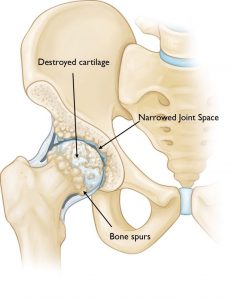
Hip Strains
Hip Strains Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Injury to the muscles that surround the hip joint.
The hip joint has various muscles surrounding the joint space providing the hip with stability and motion. When one or more of the muscles is stretched beyond its limits, it can become injured or torn causing pain, swelling, weakness and limited motion. Strains can range from mild to severe. Mild muscle strains can often be treated conservatively with rest, heat and anti-inflammatory medication. Moderate and severe muscle strains may require a more specified treatment course with physical therapy or a home exercise program to help strengthen the muscles that support the hip. It is rare that surgical intervention is needed when treating muscle strains. One can expect a recovery period of about 10 to 14 days for mild to moderate strains and longer for more severe strains. The best way to prevent muscle strains is a good stretching protocol used before and after physical activity.

Hip Bursitis
Hip Bursitis Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Bursitis of the hip which becomes inflamed and irritated.
Bursae are fluid-filled jelly-like sacs that act as cushions between bone and soft tissue for many joints throughout the body, most notably the shoulder, elbow, hip, knee and heel. When this area is irritated, it can become inflamed, causing localized pain, better known as bursitis. Typically, this is caused by repetitive stress or overuse, acute injury to the area, history of surgery to the joint, bone spurs or calcium deposits in the tendons surrounding the bursa causing irritation. Symptoms present as pain worsened with continued repetitive motion, when resting on the affected side and at night.
There are two major bursae in the hip that typically become irritated. The first one can be found over the greater trochanter, also known as trochanteric bursitis, where pain is usually felt at the outside of the thigh area. The second one is located inside of the hip joint close to the groin, commonly referred more generally as hip bursitis, and pain is often felt at the affected sided groin. A clinical exam in the office is often all that is needed for a diagnosis. Initial treatment for hip bursitis is often noninvasive and includes lifestyle modifications, NSAIDs and physical therapy. Sometimes a simple cortisone injection to the bursa is used for immediate, and sometimes permanent, relief. Surgical intervention is rarely ever needed for hip bursitis. Prevention is key when hoping to avoid bursitis. Some modifications one can do to avoid this would be weight loss, avoiding repetitive activities that put stress on the hips, and maintaining strength and flexibility of the hip muscles.
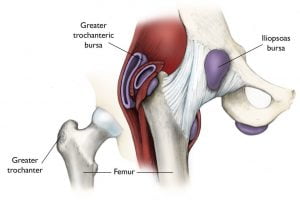
Sciatica
Sciatica Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Nerve compression at the lumbar spine causing pain, and sometimes numbness, to the
lower back which radiates to the hips, buttocks and down the back of the legs.
Sciatica is a relatively common condition that causes pain and burning along the path of the sciatic nerve — typically from the lower back which radiates to the hips, buttocks and down the back of the legs. This is most commonly due to a protruding (herniated) disk, a bone spur on the vertebrate or narrowing of the lumbar spine (spinal stenosis), all of which can compress the nerve roots that make up the sciatic nerve. Symptoms of sciatica include pain, a burning sensation and sometimes numbness along the sciatic nerve distribution route. The pain can present in varying degrees, from a mild ache to a sharp “knife-like” burning sensation. Usually only one side of the body is affected. Risk factors for developing sciatica include age, obesity, prolonged sitting, occupations that require frequent twisting or carrying heavy loads, and some conditions like diabetes and pregnancy. Sciatica is almost always treated conservatively (See our “Treatments” section for more sciatica treatment information). You should see your doctor if the symptoms persist, if the pain is severe and numbness or weakness present in your leg, or if you have trouble controlling your bowels or bladder.

Knee
Conditions & Procedures
Supracondylar/Condylar CRPP
Supracondylar/Condylar CRPP in Wayne, Parsippany & Paramus, NJ
Elbow fractures treated with wires and screws in addition to a cast.
Supracondylar/Condylar CRPP (Closed Reduction Percutaneous Pinning)
If a pediatric elbow fracture is displaced, surgery may be recommended to realign the bone and hold it in place with wires or screws in addition to a cast. The patient would then be followed closely in the office with serial x-rays to ensure bone alignment is maintained. Wires that are used to help realign the bone are typically removed in the office several weeks after surgery. If screws are utilized, sometimes these will need to be removed several months later with an additional surgery to allow for continued bone growth. Children generally regain their motion and strength without therapy, but in some cases physical therapy may be utilized.
Anterior Cruciate Ligament (ACL) Injury
Anterior Cruciate Ligament (ACL) Injury Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
ACL injuries are common injuries and create instability of the knee.
The ACL (anterior cruciate ligament) is one of the most commonly injured ligaments in the body. The ACL is found within the knee joint between the thighbone (femur) and shinbone (tibia) and acts to help stabilize the knee. Injured ligaments are considered “sprains” and are graded using a severity scale where a Grade 1 Sprain is a mildly damaged ligament to a Grade 3 Sprain where the ACL is completely torn. ACL injuries are acute injuries occurring from direct contact to the knee, a rapid direction change (i.e. pivot), sudden stopping or landing incorrectly from a jump. Patients will often feel immediate pain and experience swelling over the first 24 hours after the injury. Often the initial pain and swelling will resolve if ignored, however instability to the knee is often persistent and over time this instability can cause other posttraumatic conditions like damage to the meniscus or arthritis. A thorough physical examination can often diagnose this condition, although your doctor may order an MRI to confirm the diagnosis. Treatment for ACL injury depends on the severity and the patient’s individual needs. Nonsurgical treatment with bracing and physical therapy may be used for those with low-grade injuries, older individuals or those with very low activity levels. Otherwise, ACL tears are often surgically reconstructed using either an autograft (graft created from your own tissue) or allograft (cadaver graft) (See our “Treatments” section for more information). A personalized physical therapy program will play a vital role in rehabilitation and return to normal function of the knee after ACL reconstruction surgery.

Jumper's Knee
Jumper’s Knee Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Jumper’s knee involves inflammation of the tendon at the front of the knee that connects the patella and the tibia.
Jumper’s knee involves inflammation of the tendon at the front of the knee that connects the patella and the tibia. This issue generally develops as an overuse injury from activities that involve running, jumping, and loading the knee. Patients will feel soreness directly over the tendon and may feel pain with squatting, running, and any kind of explosive knee movements. Rest is a very important part of recovery from patellar tendonitis. Anti-inflammatory medications can be helpful for pain relief, but should not be taken long term. A focused physical therapy can be very beneficial in the rehabilitation process as well.

Patella Fracture
Patella Fracture Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
A patella fracture is a break in the kneecap, the small bone at the front of the knee
that acts as a shield to the knee joint.
A patella fracture is a break in the kneecap, the small bone at the front of the knee that acts as a shield to the knee joint. Fractures of this nature tend to be from high-impact accidents such as motor vehicle accidents or falls directly to the knee. Patella fractures result in pain, swelling and bruising to the front of the knee, an inability to straighten the knee and difficulty walking immediately following the injury. Your doctor will perform a thorough physical exam and obtain an x-ray to confirm the diagnosis and evaluate the extent of the fracture. The type of fracture will dictate the type of treatment your doctor will implement. If the fracture is stable and the articular side of the patella (the bottom part of the kneecap that glides on femur) stays in anatomic alignment, conservative treatment by immobilizing the knee is used to allow the fracture to heal appropriately. This process takes approximately six weeks before rehabilitation therapy can begin. If a patella fracture is displaced, comminuted (in many pieces) or an open fracture, it is important to surgically realign the smooth articular surface. Surgical open reduction and internal fixation (ORIF) is performed in a hospital setting using screws and/or wires in a cerclage fashion. Once the fracture has healed, a physical therapy program will help decrease stiffness, improve motion and strengthen the muscles that surround the knee.

Prepatellar (Kneecap) Bursitis
Prepatellar (Kneecap) Bursitis Treatment and Surgery in Wayne & Paramus, NJ
Prepatellar bursitis is inflammation to the bursa, a jelly-like sac that helps cushion the kneecap.
Prepatellar bursitis is inflammation to the bursa, a jelly-like sac that helps cushion the kneecap. This is most often caused by constant kneeling, often seen in patient who are plumbers, roofers, carpet layers, etc. However, repetitive direct blows to the knee (such as seen in sports like wrestling or football) can also cause prepatellar bursitis. People with rheumatoid arthritis or gout are also at risk for developing this condition. Occasionally, this condition can be caused by a bacterial infection if there is an open wound or an insect bite over the kneecap; in these cases aggressive antibacterial treatment is required. Symptoms of prepatellar bursitis include pain, swelling and redness to the front of the knee. If an infection is present, fevers and chills may accompany these symptoms. In noninfectious cases, conservative treatment with rest, ice and NSAIDs are usually all that is necessary. If infection is suspected, your doctor may aspirate the fluid to test and confirm the diagnosis where surgical drainage may be necessary to clean out the infection if antibiotics aren’t effective. Most individuals in occupations or sports that cause repetitive stress to the knees can help prevent this condition by using kneepads and practicing activity modifications when working.
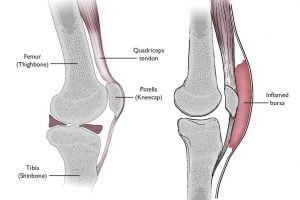
Quadricep Tendon Rupture
Quadricep Tendon Rupture Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
A tear of the quadricep tendon, the large tendon that attaches the four quadricep muscles in the thigh to the top of the kneecap.
The quadricep tendon is the large tendon that attaches the four quadricep muscles in the thigh to the top of the kneecap (patella). Quadricep tendon tears are less common than patella tendon tears, but when they do occur they are seen most often in middle-aged adults who participate in physical activity like running or jumping sports. Tendon tears are classified as either partial or complete tears. A partial tear means that there are some fibers still connected to their points of origin. A complete tear, or rupture, of the quadricep tendon is a disabling injury where the tendon is split into two pieces. These injuries are often caused by an awkward landing from a jump where a heavy load is placed on the leg with the foot planted and the knee partially bent. There are also some disease states that can weaken the patella tendon leaving it at risk for tears. Examples include tendinitis, diabetes and chronic renal failure to name a few. Steroid use like chronic corticosteroids and anabolic steroid use have also been known to weaken tendons in the body. Whatever the cause for the tear, the symptoms are generally the same. Complete tears are accompanied by a tearing or popping sensation followed by pain, bruising and swelling to the knee. An inability to straighten the knee is a hallmark symptom of this injury. Because the tendon is no longer attached to the quadricep muscles, your kneecap may migrate towards the thigh and you may feel a sizable indentation at the top of the kneecap where the tear occurred. A thorough physical exam is often all that is necessary to make this diagnosis, but your doctor may order an x-ray to observe the location of the patella or an MRI to evaluate the extent of the tear directly. Very small partial tears are good candidates for a nonsurgical treatment approach. This is accomplished by a period of immobilization to allow the tendon to heal followed by a period of physical therapy to restore strength and range of motion of the knee. If the partial tear is larger or the tendon is completely ruptured, surgery is necessary to reattach the torn tendon to the top of the kneecap (See “Quadricep Tendon Repair” under the Treatments section for more information). This is done in either an ambulatory surgical center or a hospital setting. Recovery time for this type of injury can take approximately four months and up to one year for more severe injuries.

Patella Tendon Rupture
Patella Tendon Rupture Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
A tear of the patella tendon, the tendon that attaches to the bottom of the kneecap and helps to straighten the knee.
The patella tendon is a large tendon that attaches to the bottom of the kneecap (patella) and the top of the shinbone (tibia); it works with the muscles and other tendons in the front of the thigh to straighten your leg. Tendon tears can either be a partial tear or a complete tear. A partial tear means that there are some fibers that are still connected to their points of origin. A complete tear, or rupture, of the patella tendon is a disabling injury where the tendon is split into two pieces. These injuries often require a very strong force to tear this large tendon. Some examples are direct falls to the front of the knee or landing with a very bent knee from a jump. There are also some disease states that can weaken the patella tendon, leaving it at risk for tears such as tendinitis, diabetes and chronic renal failure to name a few. Steroid use like chronic corticosteroids and anabolic steroid use have also been known to weaken tendons in the body. Whatever the cause for the tear, the symptoms are the same. Complete tears are accompanied with a tearing or popping sensation followed by pain, bruising and swelling to the front of the knee. An inability to straighten the knee is a hallmark symptom of this injury. Because the tendon is no longer anchored to the shinbone, your kneecap may migrate towards the thigh and you may feel a sizable indentation at the bottom of the kneecap where the tear occurred. A thorough physical exam is often all that is necessary to make this diagnosis, however your doctor may order an x-ray to observe the location of the patella or an MRI to evaluate the extent of the tear directly. Very small partial tears are good candidates for a nonsurgical treatment approach. This is accomplished by a period of immobilization to allow the tendon to heal followed by a period of physical therapy to restore strength and range of motion of the knee. If the partial tear is larger or the tendon is completely ruptured, surgery is necessary to reattach the torn tendon to the kneecap (See “Patella Tendon Repair” under the Treatments section for more information). This is done in either an ambulatory surgical center or a hospital setting. Recovery time for this type of injury can take six months or more for severe tendon injuries.

Knee Arthritis
Knee Arthritis Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Knee arthritis is a common condition where the protective cartilage in the knee joint is worn down and the protective space between the bones decreases.
Knee arthritis is a common condition where the protective cartilage in the knee joint is worn down and the protective space between the bones decreases. This results in bone rubbing on bone, producing irritation and painful bone spurs. The most common type of arthritis is osteoarthritis, caused by chronic wear and tear of the joint. Rheumatoid arthritis is an autoimmune disease where the immune system attacks normal tissue and often effects multiple joints in the body. Posttraumatic arthritis develops after an injury to the knee where change to the joint surface can have long term arthritic effects. Symptoms of knee arthritis include pain and swelling to the knee joint, stiffness, weakness, and a grinding or locking sensation. This diagnosis is often made in our office with a thorough physical exam and x-rays. There is no cure for arthritis and therefore treatment is centered around symptom relief often in the form of lifestyle modifications, physical therapy, NSAIDs, braces and/or cortisone injections. In cases of rheumatoid arthritis, immunosuppressant medication may be prescribed. We also offer hyaluronic acid injections (i.e. Synvisc, Orthovisc) to help alleviate knee arthritis symptoms; these injections are a viscous gelatinous substance that helps increase lubrication in the joint. If conservative treatment does not help and daily living is affected, a partial or total knee replacement (arthroplasty) may be indicated. Please see our “Treatments” section for more information on knee arthroplasty.

Baker’s Cyst
Baker’s Cyst Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
A Baker’s cyst is a swelling at the back of the knee caused by outpouching of the normal synovial fluid found in the knee joint.
A Baker’s cyst, also known as a popliteal cyst, is a swelling at the back of the knee caused by outpouching of the normal synovial fluid found in the knee joint. They are usually visible as a soft bulge behind the knee and are more prominent when standing. Normally, these cysts do not cause symptoms and are nontender. However, knee stiffness or pain can occur especially when the knee is in full extension. Knee arthritis is the most common cause of Baker’s cysts, but these cysts can also occur when associated with injury to the knee such as meniscal tears. These cysts usually do not need any formal treatment, especially if they do not cause any discomfort. If the cyst is associated with pain and discomfort, your doctor may perform an ultrasound-guided aspiration to drain the cyst. Sometimes just draining the cyst is not a definitive treatment, and these cysts can recur. In these cases, a more formal surgical approach may be indicated to completely resolve the source of the cyst (i.e. knee arthroscopy, please see “Knee Arthroscopy” under our Treatments section for more information on this). It is not uncommon for a Baker’s cyst to rupture on its own, leaving a painless bruising under the skin usually seen down at the level of the ankle.

Collateral Ligament Injuries
Collateral Ligament Injuries – Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
The collateral ligaments of the knee are the MCL (medial collateral ligament) and the LCL (lateral collateral ligament).
The collateral ligaments of the knee are the MCL (medial collateral ligament) and the LCL (lateral collateral ligament). These ligaments are found on the sides of you knee joint — the MCL connects the thighbone (femur) to the shinbone (tibia) whereas the LCL connects the thighbone (femur) to a smaller bone in the lower leg (fibula). These ligaments together control sideways motion and brace the knee against unusual movement. Injuries to these ligaments are graded where a Grade 1 Sprain is a mild injury and a Grade 3 Sprain is a complete tear. These injuries are often caused by unusual sideways force to the knee. The MCL is more commonly injured than the LCL, usually from blows to the outside of the knee forcing the knee inwards. Pain, swelling and instability are the predominant symptoms associated with these injuries. A thorough physical exam will help make this diagnosis, but an MRI may be obtained to visualize the extent of the injury. MCL injuries rarely require surgery and are often treated with rest, ice, NSAIDs, bracing and physical therapy. If the collateral ligaments are torn in a way that does not promote healing or in conjunction with other ligamentous injuries, reconstructive surgery may be indicated. Progressive rehabilitative therapy will be an important part of the recovery process.
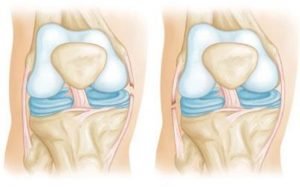
Meniscus Tear
Meniscus Tear – Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Injury to the meniscus, which is a wedge-shaped cartilage disc in the knee that cushions and absorbs shock.
The meniscus is a wedge-shaped cartilage disc in the knee that cushions and absorbs shock between the femur (thighbone) and tibia (shinbone). Meniscus tears can occur acutely from direct contact or a twisting injury, or they can occur due to degenerative changes over time. Symptoms include pain, swelling, stiffness, a catching or locking sensation, weakness, or a “giving way” sensation. Your doctor can often make this diagnosis in the office but may order some advanced imaging such as an MRI to visualize the location and extent of the tear. Conservative treatment typically consists of the RICE protocol (rest, ice, compression, elevation), NSAIDs and/or physical therapy. If your symptoms persist or the knee is unstable, surgical intervention to either debride or repair the affected meniscus may be necessary. See our “Treatments” section for more information.
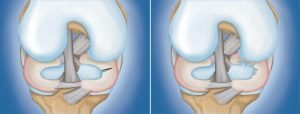
Patellofemoral Syndrome
Patellofemoral Syndrome – Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Patellofemoral syndrome, aka “runner’s knee”, is a painful condition affecting the front of the knee.
Patellofemoral syndrome, aka “runner’s knee”, is a painful condition to the front portion of the knee. Often this condition occurs in young adults who participate in regular activity like sports or running, but pain to the anterior portion of the knee can occur in older individuals and nonathletes as well. Usually this is caused by overuse of the knee and/or problems with the alignment of the kneecap. Pain to the front of the knee is often the most common symptom. Pain with this condition often occurs during activity, especially activity involving repeatedly bending the knee or after prolonged sitting. Your doctor will do a thorough exam to determine if this diagnosis is due to overuse or kneecap malalignment. Conservative treatment is recommended as first-line therapy. This includes the RICE protocol (rest, ice, elevation, compression), NSAIDS, and lifestyle medications and physical therapy. Sometimes arthroscopic surgery may be needed to in cases where the kneecap is misaligned. Prevention is key to avoid patellofemoral syndrome — wearing appropriate footwear when participating in activity, stretching before and after exercise, and maintaining a normal body weight to avoid stress to the knees are all effective preventative measures.

Pediatric Orthopaedics
Conditions & Procedures
Pediatric Elbow Fractures
Pediatric Elbow Fractures: Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Elbow Fractures
There are three bones that make up the elbow joint and allow you to bend and straighten your arm and turn your palm up and down.
Since children’s bones are still growing, bone fractures in children are unique. Without proper diagnosis and treatment of pediatric fractures, patients can experience future complications. We work with children to make sure their bone fractures are diagnosed and treated correctly so they heal properly.
Pediatric Forearm and Wrist Fractures
Pediatric Forearm and Wrist Fractures: Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Forearm and Wrist Fractures
The forearm is made up of two bones from your elbow to your wrist called your radius and ulna and can break anywhere along their length. Sometimes only one of the bones is broken and other times both bones break. Fractures near the wrist may be associated with a break through or near the growth plate.
Since children’s bones are still growing, bone fractures in children are unique. Without proper diagnosis and treatment of pediatric fractures, patients can experience future complications. We work with children to make sure their bone fractures are diagnosed and treated correctly so they heal properly.
Pediatric Femur (Thigh Bone) Fractures
Pediatric Femur (Thigh Bone) Fractures: Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Femur (Thigh Bone) Fractures
The femur, or thigh bone, is the largest bone in the body. The top of the femur connects to the pelvis to form the hip joint and the bottom of the femur connects to the tibia or shin bone to form the knee joint.
Since children’s bones are still growing, bone fractures in children are unique. Without proper diagnosis and treatment of pediatric fractures, patients can experience future complications. We work with children to make sure their bone fractures are diagnosed and treated correctly so they heal properly.
Pediatric Ankle Fractures
Pediatric Ankle Fractures: Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Ankle Fractures
The ankle is a common location for breaks in children. The ankle joint is made up of three bones: the tibia (shin bone), the fibula (smaller bone on the outside of the leg) and the talus (bone beneath the shin bone).
Since children’s bones are still growing, bone fractures in children are unique. Without proper diagnosis and treatment of pediatric fractures, patients can experience future complications. We work with children to make sure their bone fractures are diagnosed and treated correctly so they heal properly.
How To Care For Your Cast
How To Care For Your Cast Tipa from Wayne, Parsippany & Paramus, NJ
Keep your cast DRY! Keep your cast CLEAN! Keep your cast COMFORTABLE!
Since children’s bones are still growing, bone fractures in children are unique. Without proper diagnosis and treatment of pediatric fractures, patients can experience future complications. We work with children to make sure their bone fractures are diagnosed and treated correctly so they heal properly.
Does My Child Need A Pediatric Surgery Specialist?
Pediatric Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Choosing a doctor to take care of your health concerns is always difficult, but when it comes to your child’s health it can be even more challenging. Modern Orthopaedics wants to help you better understand the importance of choosing an orthopaedic specialist that has been trained in pediatric care.
Small, growing bones, ligaments, and muscles are different than fully matured ones and need to be treated as such. Understanding the nuances of pediatric orthopedic care is crucial to having good outcomes following an injury or issue. Your doctor needs to recognize your child’s musculoskeletal development to treat them successfully. At Modern Orthopaedics, all our doctors have been trained in pediatric care in each of their particular specialties. This helps ensure that your child will be treated differently than an adult. Our doctors will take the time to assess how each child is maturing and develop a treatment plan accordingly.
You can put your mind at ease knowing that our doctors at Modern Orthopaedics are not only specialists in their field, but also have specific pediatric training. This training has equipped them to treat all pediatric orthopaedic problems from simple to the most complex.
Foot & Ankle
Conditions & Procedures
Achilles Tendon Rupture
Achilles Tendon Rupture – Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
A complete tear of the Achilles tendon, a large tendon that runs down the back of the leg and connects to the heel of the foot.
The Achilles is a large tendon that runs down the back of the leg and connects to the heel of the foot. This is the largest tendon found in the body and is used when walking, running, jumping, etc. While this tendon is very strong and can withstand a great deal of stress, a partial tear or rupture can still occur if that stress becomes too great (i.e. forceful jumping or pivoting, sudden accelerations or decelerations, tripping or falling). While anyone can experience an Achilles tendon rupture, these are most often seen in those who exercise infrequently (sometimes referred to as “weekend warriors”), those taking certain medications which can affect the integrity of the tendons in the body (i.e. some steroids and antibiotics), and those with Achilles tendinitis. Patients often feel a sudden snap or “pop” with immediate pain to the back of the ankle followed by swelling and difficulty walking. This injury tends to be an obvious diagnosis, but in some cases an MRI may be obtained to evaluate the degree of the tear. Surgery to repair the tendon is often performed in a timely manner to ensure optimal healing and functionality. In some cases, if the tendon is not completely torn or the patient is not an optimal surgical candidate, non-surgical treatment may be implemented. In either case, physical therapy is an important component to the overall healing process.
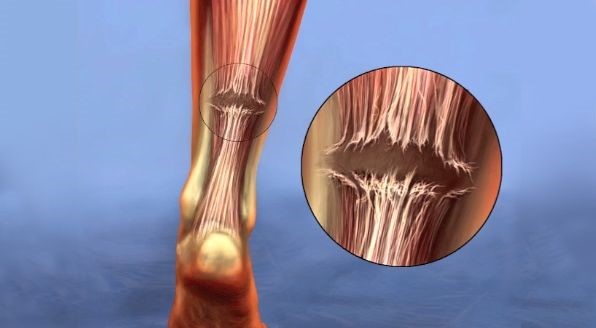
Achilles Tendinitis
Achilles Tendinitis Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Inflammation and pain to the Achilles, a large tendon that runs down the back of the leg and connects to the heel of the foot.
The Achilles is a large tendon that runs down the back of the leg and connects to the heel of the foot. This is the largest tendon found in the body and is used when walking, running, jumping, etc. With overuse and/or degeneration, this tendon can become irritated and inflamed which is commonly referred to as tendonitis. Sometimes bone spurs can form at the heel bone (calcaneus). This condition usually develops from repetitive stress to the tendon, sudden increased intensity during exercise or other physical activity, calf muscle tightness and bone spurs. You may feel pain and stiffness along the tendon, pain that worsens with activity, thickening of the tendon, soft tissue swelling around the area, and a decreased range of motion of the ankle. Achilles tendinitis leaves the Achilles tendon vulnerable to Achilles tendon ruptures (see more on this under our “Conditions” section). Imaging usually isn’t necessary for a diagnosis; however, an x-ray may show bone spurs at the calcaneus if degenerative changes are present. Treatment is often conservative with rest, ice, NSAIDs and physical therapy focusing on stretching exercises, but it may take several months before symptoms improve. Prevention is key when avoiding this condition — stretching calf muscles before and after physical activity and wearing the correct footwear.

Ankle Fractures
Ankle Fractures – Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
An ankle fracture is a break in one or more of the bones that form the ankle joint.
There are three bones that make up the ankle joint: the tibia (shinbone), the fibula (smaller bone of the lower leg) and the talus (bone found between the heel bone and the tibia/fibula). There are also multiple ligaments found at the ankle joint that help keep the ankle stable. When speaking in terms of ankle fractures there are three boney areas that we refer to: the medial malleolus (the inside protrusion of the tibia that we associate with the ankle), the lateral malleolus (the outside protrusion of the fibula that we associate with the ankle) and the poster malleolus (the back part of the tibia). Ankle fractures are classified according to the area of the bone that is broken (i.e. medial malleolus fracture). If two of these malleoli are broken, we refer to this as a bimalleolar fracture. Bimalleolar fractures most often include the medial and lateral malleoli. Trimalleolar fractures involve a fracture to all three of the malleoli. The severity of the fracture involves the number of breaks that have occurred, stability of the ankle joint and if ligamentous injury is present. The most common ligamentous injury seen with ankle fractures is a syndesmotic injury. The syndesmosis joint can be found between the two bones of the lower leg (tibia and fibula) which are held together by ligaments (for isolated syndesmotic injuries, please see “Ankle Sprains” in our “Conditions” section). Ankle fractures can be caused by direct impact to the area, twisting or rotating the ankle, “rolling” the ankle, or tripping/falling. Symptoms can include severe and immediate pain, bruising, swelling, tenderness, inability to bear weight or an obvious deformity. X-rays are often the first imaging tool when diagnosing an ankle fracture and its severity. Nonsurgical treatment may be utilized by your doctor if the ankle remains stable and the fractured bones are still in anatomic alignment or if the patient is not a surgical candidate. In these cases, a CAM boot or a cast will be applied and non-weight bearing measures are taken to allow the fracture to heal. Serial x-rays are then used to ensure proper fracture healing occurs. If the fracture is more severe where displacement has occurred, the ankle joint is unstable, dislocation of the ankle joint is present, multiple bones are involved or ligamentous injury is present, surgical intervention with hardware placement may be required (see “Ankle ORIF” for more information)
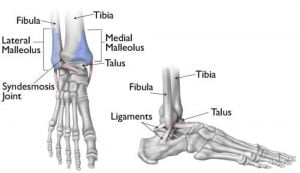
Ankle Fusion
Ankle fusion surgery is a procedure offered by Modern Orthopaedics of New Jersey that joins the foot bone to the leg bones to alleviate pain and improve foot function. It’s usually considered when other treatments fail to relieve symptoms. The surgery, which can be done through an anterior/lateral approach or arthroscopically, involves aligning the bones and securing them with hardware. Pre-surgical preparation includes a health review and imaging tests. Post-surgery, patients use splints and assistive devices to avoid weight-bearing and undergo physical therapy to adjust to the immobilized joint. Recovery typically takes about four months. Risks include pain, swelling, and potential complications, but these are generally low. Costs vary by insurance coverage, and the procedure is usually insured when medically necessary. Alternative therapies and surgeries are available and discussed before opting for fusion. For more information on recovery, risks, and alternatives to ankle fusion, contact Modern Orthopaedics of New Jersey.
Ankle Sprains
Ankle Sprains – Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Ankle sprains are the most commonly seen sports injuries; however, ankle sprains can happen among people of all ages and activity levels.
Ankle sprains are the most commonly seen sports injuries; however, ankle sprains can happen among people of all ages and activity levels. When the term “sprain” is used, it refers to an injury to a ligament, the tough fibrous connective tissue found between two bones. There are many ligaments around the ankle joint that help with motion and stability. When one of these ligaments around the ankle are injured, bleeding and swelling occur. This is the body’s response to heal an injured area. Ankle ligaments often do heal on their own due to the increased blood that travels to the area. Swelling and bruising are usually more pronounced at the ankles due to this response, and the distance of the ankles from the heart can cause the ankles to remain swollen for prolonged periods following the injury. Most mild to moderate ankle sprains (Grade 1 and Grade 2 respectively) can be treated at home with the RICE protocol (rest, ice, compression and elevation) and NSAIDs (nonsteroidal anti-inflammatory drugs). You should see your doctor if the sprain is severe (Grade 3), the pain is severe when bearing weight or you can’t walk at all. Nonsurgical treatment is commonly implemented first, often using a brace or a CAM boot to immobilize the joint appropriately and allow for adequate healing. If extensive tearing of the ligament(s) is expected after a clinical exam, an MRI may be ordered. The American Academy of Orthopaedic Surgeons suggests a three-phase program for all ankle sprains when treated conservatively:
– Phase 1: resting, protecting the ankle and reducing the swelling.
– Phase 2: restoring range of motion, strength and flexibility. Physical therapy is often utilized here to prevent stiffness and increase ankle strength.
– Phase 3: maintenance exercises and the gradual return to activities that do not require turning or twisting the ankle. Eventually, activities that require more intense activities that require sharp, sudden turns (i.e. tennis, basketball) can be reintroduced.
The length of this treatment program may take just two weeks to complete for minor sprains, or up to six to 12 weeks for more severe sprains. Surgical treatment for ankle sprains is rare; however, it is sometimes necessary for severe injuries that fail to respond to nonsurgical treatment. High ankle sprains (also known as syndesmotic injuries) sometimes require surgical intervention with a “tightrope” or a screw if the syndesmotic joint (joint found between the tibia and fibula) is found to be unstable. As with many other conditions, prevention is the best way to avoid ankle sprains. This includes using caution when walking or running on uneven surfaces, wearing proper footwear, and implementing a thorough warm up and stretching regimen before and after physical activity.
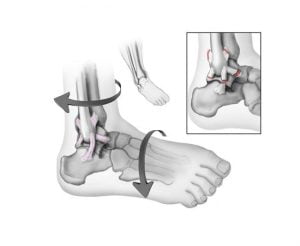
Arthritis of the Foot and Ankle
Arthritis of the Foot and Ankle – Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Rheumatoid arthritis is a type of autoimmune disease that tends to effect multiple joints in the body simultaneously but often starts in the foot and ankle and usually affects both sides of the body (symmetrical presentation)
There are 28 bones in the foot and ankle and more than 30 joints that provide a wide range of movement, support and shock absorption. Arthritis of any one or many of these joints can cause pain, stiffness and difficulty performing physical and daily activities if these symptoms become severe. The most common type of arthritis seen is osteoarthritis, or a degeneration (wear and tear) of joint. This condition occurs gradually and certain risk factors can increase your risk of developing osteoarthritis: advanced age, obesity, laborious occupations, a high level of physical activity or previous trauma to the joint (also known as posttraumatic arthritis). Rheumatoid arthritis is a type of autoimmune disease that tends to effect multiple joints in the body simultaneously but often starts in the foot and ankle and often effects both sides of the body (symmetrical presentation). Symptoms of foot and ankle arthritis are pain with motion, flare ups with activity, swelling and/or redness over the affected joint, difficulty walking due to pain, and tenderness with applied pressure to the area. X-rays are often used by your doctor to help visualize the joint(s) involved. Joint space narrowing and bone spurs are common findings on x-rays. Sometimes blood tests, specifically in rheumatoid arthritis cases, are required to help confirm a diagnosis. While there isn’t any cure for arthritis, there are some treatment options that our doctors may recommend: lifestyle modifications, physical therapy and NSAIDs are often first-line therapy options. Sometimes supportive braces are utilized as well. If a patient’s arthritis is severe and symptoms effect daily activity, surgery may be recommended. Arthroscopic debridements can be performed to remove loose cartilage, inflamed synovial tissue and bone spurs from the affected joint space. More invasive surgical options include an arthrodesis (complete fusion of the joint with hardware or screws) or a joint arthroplasty (replacement of the affected joint with prosthetics). While surgery can be very effective in relieving arthritis pain, it is usually reserved only for more severe cases.

Bunion Surgery
Bunion surgery at Modern Orthopaedics of New Jersey corrects the painful deformity of the big toe known as hallux valgus. It’s recommended for patients with significant pain after conservative treatments have failed. The process begins with a thorough evaluation of the patient’s condition through physical exams and X-rays, followed by a detailed discussion of surgical options, including fusion, osteotomy, exostectomy, and joint space-producing procedures. Preoperative assessments and discussions about the patient’s overall health, risks, and recovery expectations precede the elective procedure. Post-surgery, patients will follow a specific care plan, including medication, protective dressings, limited weight-bearing, and eventual physical therapy to ensure successful recovery and return to daily activities. Costs vary based on insurance coverage, but most plans cover necessary surgical corrections. Alternative non-surgical therapies are also available. For further details on bunion treatment and surgery, contact Modern Orthopaedics of New Jersey.
Lisfranc Injury
Lisfranc Injury – Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
A Lisfranc injury is an injury of the midfoot that involves either a break to the bones and/or a strain to the ligaments that connect the midfoot to the forefoot.
A Lisfranc injury is an injury of the midfoot that involves either a break to the bones and/or a strain to the ligaments that connect the midfoot to the forefoot. Lisfranc injuries can result from direct trauma (i.e. a fall from a height) or from a twist-and-fall scenario, often seen when someone stumbles over the top of a foot that is flexed downward. Symptoms include swelling and pain to the top of the foot, bruising to the top and bottom of the foot, and pain worse with standing, walking or pushing off the affected foot. These injuries can be easily confused as a simple sprain, but given the location, these injuries are considered severe and must be treated appropriately. If a Lisfranc injury is suspected, your doctor may order advanced imaging to evaluate for any fractures or ligament tears. Nonsurgical treatment is always the goal and can sometimes be achieved if the injury is not severe and no fractures, joint dislocations or complete ligamentous tears are present. A cast or boot would be applied and a strict non-weight bearing regimen for six weeks (or longer) would be enacted to allow proper healing. However, in most cases this injury requires surgical repair, often with screws and plates which would later need to be removed once the injury has fully healed.
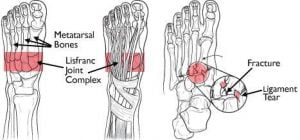
Morton’s Neuroma
Morton’s Neuroma – Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
A Morton’s neuroma is a thickening of the tissue that surrounds the digital nerve that goes to the toes.
A Morton’s neuroma is a thickening of the tissue that surrounds the digital nerve that goes to the toes. This condition creates a persistent pain at the ball of the foot and is often described as a “walking on a marble” sensation. The most frequent location is between the third and fourth toes. Women are more likely to develop the condition than men. This diagnosis can be made easily in the office setting and treatment is often nonsurgical with proper footwear recommendations or orthotics; sometimes cortisone injections can help relieve the symptoms.

Plantar Fasciitis
Plantar Fasciitis Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
Inflammation of the plantar fascia, a long ligament found at the bottom of the foot which connects your heel to the front of your foot and helps support the foot’s arch.
The plantar fascia is a long ligament found at the bottom of the foot which connects your heel to the front of your foot and helps support the foot’s arch. The foot is made to withstand high amounts of pressure and movement, however sometimes too much pressure on the plantar fascia can cause damage and tears resulting in an inflamed and irritated plantar fascia or “fasciitis.” This usually develops over time and many factors can contribute to this progressive condition: obesity, high foot arches, repetitive impact activities or tight calf muscles to name a few. Patients usually complain of pain at the bottom of the foot, especially the first few steps after getting out of bed in the morning and after exercise. This is a clinical diagnosis, however if x-rays are obtained it is common for your clinician to see a bone spur at the heel bone (calcaneus). Treatment is almost always conservative with rest, ice, NSAIDs, stretching exercises, and wearing proper footwear or orthotics. Sometimes cortisone injections may be used to reduce inflammation and pain. Electrocorporeal shockwave therapy (ESWT) has been used to help stimulate the healing process of the damaged fascia (See “Electrocorporeal shockwave therapy” for more information).
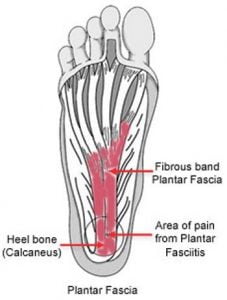
Toe and Forefoot Fractures
Toe and Forefoot Fractures – Treatment and Surgery in Wayne, Parsippany & Paramus, NJ
A break in one or more of the 29 bones found in the foot.
The foot is comprised of many bones: the forefoot alone has 29 bones — five metatarsal bones and 14 phalanges (toe bones). A break in any of these bones can be very painful and make walking a difficult task. Most acute fractures in the foot occur from direct force (like dropping a heavy object onto the foot) or trauma (like kicking a hard object). “Stress” fractures are small fractures that can also develop over time due to repetitive activity. Fractures in the foot usually cause bruising to the top and bottom of the foot, swelling and pain, especially when walking or bearing weight. An x-ray is used to evaluate the injury and determine the location, type and severity of the fracture. Fractures of the toe (phalangeal bones) are the most likely bones of the foot to fracture. Toe fractures, while painful, often do not need any surgical treatment. Allowing the fracture to heal with rest and supportive shoes are usually appropriate first-line care for most toe fractures. Metatarsal fractures are breaks in the long bones found in the middle of the foot. Like toe fractures, these fractures can be treated with a period of rest, ice, elevation, and supportive shoe wear or a brace. However, if there are several metatarsal fractures involved, concurrent ligamentous injury, and the foot is deformed or unstable, an open reduction with internal fixation (ORIF) with plates and/or screws may be necessary to regain proper function and mobility of the foot (Please visit out Treatments section for more information of toe and forefoot fracture treatment). Your doctor will monitor the fracture closely with serial x-rays during your treatment course to ensure proper alignment of the bone is maintained throughout the healing process.