I think I might have a torn rotator cuff. What should I do?
If you think you have a rotator cuff tear, book an appointment with an Orthopaedic Specialist who specializes in diagnosing and treating shoulder injuries.
A true specialist can identify the underlying cause of your pain. Generally, the cause is a cuff tear or another problem, such as a SLAP tear, tendonitis, arthritis, or bursitis .A sports medicine specialist can provide comprehensive care for rotator cuff injuries, from diagnosis to rehabilitation.
Solving these types of injuries starts with an accurate diagnosis and treatment plan, and most likely an imaging study will be needed.
The first imaging tests performed are usually X-rays. X-rays do not show the soft tissues of your shoulder (like the rotator cuff). Many doctors will want to see these imaging results to make sure you don’t have other reasons for your shoulder pain, such as arthritis, a bone spur, etc.
The second imaging test commonly performed is Magnetic resonance imaging (MRI) or ultrasound. An MRI can better show soft tissues, like the rotator cuff tendons, than an X-ray. A tear in the rotator cuff tear is usually visible in an MRI of the shoulder, as well as where the tear is located within the tendon and the size of the tear. An MRI can also give your specialist a better idea of how old or new a tear is because it can show the quality of the rotator cuff muscles.
If you’re experiencing symptoms of a torn rotator cuff, don’t suffer in silence. Contact our orthopedic surgeons in Wayne, NJ today to get the relief you need.
Video Transcript
Rotator Cuff Syndrome Overview
All right, rotator cuff syndrome. Now, what is that? That’s sort of like a umbrella term for anything any disorder related to the rotator cuff. And what is the rotator cuff? It’s commonly heard in general out there in the community. My rotator cuff hurts or something like that. And it may be because it’s a very, very important, complex, and often injured structure of the shoulder.
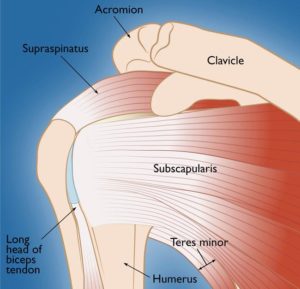
There’s four tendons that make up the rotator cuff and one of them is responsible for internal rotation called the subscapularis tendon. The other three are on the top end angling towards the back and are more responsible for external rotation and also holding the joint stable. And it is a really nice system. It allows stability of the shoulder in addition to allowing for all this motion and rotation and elevation and going behind your back.
So all that stability we enjoy is brought to you by and control is brought to you by the rotator cuff. And at times, especially as we get older, those tendons can get a bit worn or pinched or kind of degraded in a way. And as the same amount of force gets put through them and if the tendon degrades a little bit, you start to get degenerative changes within the tendon. And that actually can cause it can be a pain generator. can cause pain.
What Is Rotator Cuff Syndrome?
The type of pain that you might expect when you have a rotator cuff tear or a rotator cuff, we’ll call it tendinopathy or disease of the tendon tissue is pain right on the outside of your shoulder. Sometimes it radiates down into the outside of your shoulder as well over towards the lateral aspect of your arm. It can go down the front of your arm.
And it’s very often that if you elevate your arm at or above your eye level, that can be a symptom or sign of rotator cuff pathology or problem. Also, this is a very common symptom, but having it disrupt your ability to sleep at night. Some people I always ask patients, does it affect your ability to sleep or does it wake you up from sleep? And that’s a big problem obviously if you’re waking up from sleep and can’t get a good night’s sleep because of your shoulder pain. that brings a lot of patients into my office and it’s one of the reasons, one of the few reasons why I sometimes consider cortisone injections in this scenario.
Symptoms and Pain Characteristics
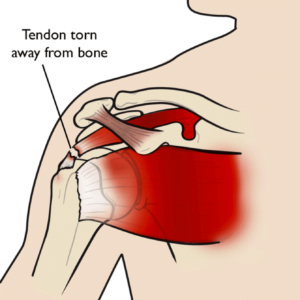
But then the issue is how do we evaluate and treat rotator cuff pathology? First, we got to figure out is it a painful rotator cuff that is intact or is it a rotator cuff that has a partial or even a full thickness tear where it’s now tearing away from the top of the bone. And if that’s the case, then we have to start tailoring our treatments.
First and foremost, often times if it’s at traumatic rotator cuff pathology, physical therapy is sort of the mainstay of treatment. Now, if that’s not good enough after four or 6 weeks of comprehensive therapy, and by the way, about, you know, 70 to 80% of the time, that will be effective for you. That’s why we start with therapy.
But in the cases that where the pain persists or isn’t feeling well enough then I’ll get it usually get an MRI at that point and in order to sort of evaluate the anatomy of the rotator cuff and then we can look for things like tears tendonopathy which again means the tendon is intact but the tendon quality is a little bit degraded and those are all things that could be associated with the pain that you’re feeling.
How Do We Evaluate and Treat Rotator Cuff Pain?
Once I have a sense of that, then we can either continue therapy or potentially offer other treatment options. In other videos, we’ve talked about things like platelet rich plasma, which can be a regenerative option to help tendon tissue improve its quality and decrease the pain.
Now, if you have a rotator cuff tear, that’s a completely different story. and therapy still could be effective, but it’s likely to be less effective than if you just have a a tendonopathy that gets better with therapy. So, if you fail another, say, month or so of therapy, so it’s going on several months, maybe it’s still disrupting your ability to sleep, you have a rotator cuff tear to some degree, that’s when we start to discuss surgical options to actually take the tendon, retension it, and anchor it back to the bone.
And that process is very very effective at treating your pain. The downside obviously is that you have to have surgery, but it’s worth it if you just can’t sleep, you can’t function, and you can’t do the activities that you like to do. So that’s where we start talking about the risks and benefits of surgery.
I will say rotator cuff surgery is probably of all the surgeries I perform probably is the longest recovery time of all the surgeries. And those patients are very, very happy when they’re done with their recovery. But through the process, it takes time and we have to wait for the tendon to heal down to the bone and that takes at least 6 weeks to start the healing process.
And that’s where we start therapy at about 6 weeks posttop. If you’ve had pain in your shoulder that isn’t going away, consider calling Modern Ortho to help you understand what’s going on and what can be done about it.
What to Expect After Surgery
So, you’ve had rotator cuff surgery. This is what to expect post-operatively. After rotator cuff surgeries or most rotator cuff surgeries, we’ll have you in a sling. And I have my patients wear a sling pretty much for the whole time from surgery to 6 weeks posttop.
And in that period of time, they are allowed to move the elbow out of the sling and take it off for showers. And usually most patients, I’ll have them do some pendulum exercises where they lean forward. It kind of gravity then takes the arm forward a little bit. They can do a little bit of motion, but that’s just about it. I don’t want any kind of force actually on the repair.
So that allows some early motion but very very limited. It’s really about rest at that point. The construct that we use even though it’s anchors in the bone that that are attached to sutures that hold the tendon down onto the bone that’s strong but not strong enough and we can very easily overcome that if we start elevating our arms.
So those are the early instructions. Now at 6 weeks post-operatively you have some very early healing that allows us to start the therapy at that point. So, I usually get you in with a good therapist who can carry out our rehab protocol. And that’s going to be from 6 weeks to 12 weeks.
We’re going to have you doing active assisted range of motion where we’re going up and and trying to explore all the depths of motion, elevation, external rotation, internal rotation, and also just, you know, massaging the surgical scars, the portal sites that we do because we do this all through an arthroscopic approach.
So after that at 3 months posttop is when we start doing some of the strengthening. Very very light stuff that we start. And from about 3 months to 6 months is really where you start to see your strength start to improve and the comfort levels improve and the range of motion all the while is also improving to the point where now you’re sleeping through the night.
You’re feeling better. The pain that you had prior to surgery is gone. You have some improving postoperative pain. And I always tell my patients that have to go through these operations and they’re very happy at the end of the course, but that ultimately the majority of the result like your final final result will be after 1 year.
So, you know, it’s an investment in your time to get past something that just isn’t getting better through other means like therapy, PRP, shockwave, maybe even a cortisone injection. So, that’s the general idea.
Final Thoughts
It is obviously a big deal to go through surgery, but it’s worth it if your problems are such that they’re disrupting your life. At Modern Orthopedics, we’re here to help you live pain-free. See you in the next video.